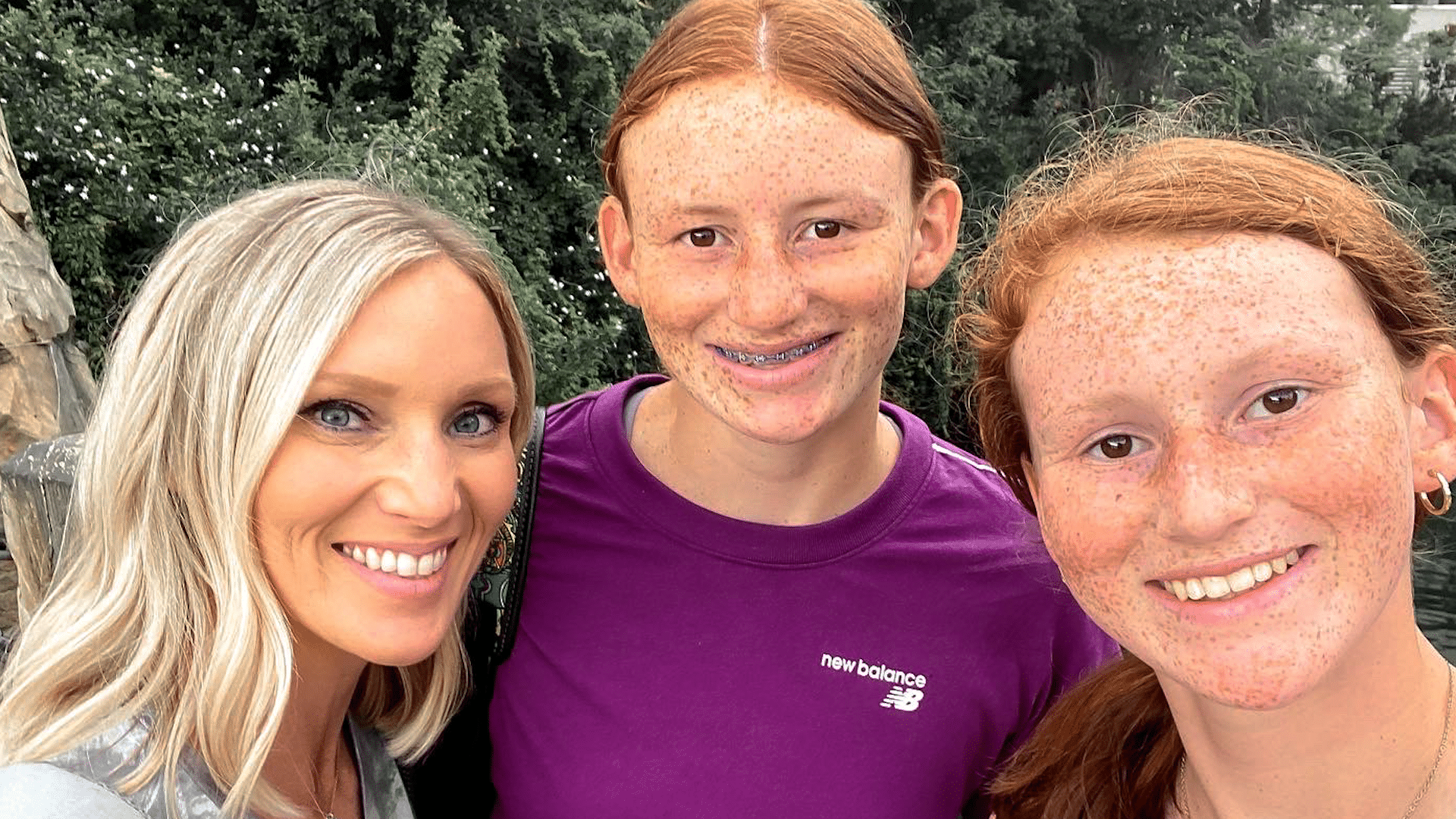
It started out as a typical holiday weekend for Dana Parker and her two daughters.
“We had plans to go hang out with my family the next day, for a cookout,” Dana said, about their plans last summer. “Fourth of July is a big holiday in our family.”
But overnight, those plans for a celebration quickly changed.
“I woke up a few times the next morning and thought, ‘Man, the house is really quiet. I’m surprised the girls aren’t up yet,’” Dana said.
Next came a horrifying discovery, as Dana found her oldest daughter Parker unresponsive on their living room floor.
“She’s just covered in vomit. She had definitely aspirated, I can hear it gurgling in her lungs,” Dana said, as she recounted the experience that day. “Her body is cold, I mean it is cold, stiff, she’s not responsive at all.”
Dana then finds herself reeling as first responders hone in on a possible cause. “They just kept saying, ‘Do you think it could be an overdose?’ They’re hooking her up to all these things and they just keep going back, like ‘Ma’am, she’s young, she’s healthy, all of these symptoms point to an overdose,’” she said.
Evidence found on Parker’s cell phone confirmed those suspicions. “In the course of about 25 minutes, she consumed almost 26 shots of alcohol,” Dana said.
“Depending on how old you are, how much you weigh, how much alcohol you’re ingesting, every child is different in terms of the effect it’s going to have on you,” Nicole Belcher, PA-C, a physician assistant at the James and Connie Maynard Children’s Hospital at ECU Health Medical Center (VMC).
In Parker’s case, she consumed enough alcohol for the care team at the Children’s Emergency Department at VMC to warn of an unknown outcome.
“They said, ‘At this point we don’t know if she’ll wake up. And if she does we have no idea what condition she’ll be in,’” Dana said. “She was already on borrowed time. I mean, it is literally by the grace of God that she was even still breathing at that point.”
Breathing then – and thriving now. While minor nerve issues persist, the multi-sport student athlete has made nearly a full recovery. And Dana is grateful for the care her daughter received.
“The little things that they do mean more than what they realize. Just the little kind words and taking the time to ask the questions and to say, ‘Hey, are you ok? Is there anything I can get you?’ I would just love to say ‘thank you,’” Dana said.
Now Dana wants other parents to learn from her family’s experience, and to consider how they talk to their children about the dangers of drinking.
“In her eyes, maybe she was drinking responsibly. She wasn’t out on the street, she wasn’t at a party, she wasn’t driving, you know – she’s in the comfort of her own home. She gets curious, she wants to experiment,” Dana said.
Experts agree.
“Bottom line, is to have the conversation. I think the earlier we walk about it, the better,” said Belcher. “The reality is, they are going to learn it from you, or they’re going to see it on social media, they’re going to see it on television, they are going to see it on the movies. Being able to have that open communication and being able to model safe behaviors with alcohol is the most important thing.”
Resources
April is Alcohol Awareness Month. If you or a loved one needs support, resources or treatment, the Substance Abuse and Mental Health Services Administration (SAMHSA) can help.
SAMHSA’s National Helpline is free, confidential and accessible 24 hours a day, seven days a week: 1-800-662-HELP.
They also offer an online treatment locator: https://findtreatment.samhsa.gov/
Watch more ECU Health News videos
On July 23, 2021, Cleere Reaves, 26 and a half weeks pregnant with her and her husband Will’s first child, headed to a regularly scheduled OB-GYN appointment with Dr. Kori Whitley for a glucose screening.
Cleere also had an ultrasound added to her visit, though it wasn’t totally necessary based on her scheduling.
“Praise God that was added,” Cleere said.
The ultrasound showed that something was wrong in the womb and it was time to move Cleere immediately over to Maynard Children’s Hospital at Vidant Medical Center. Dr. Whitley told Cleere and Will that they might be 90 hours from delivery, but their son would likely need to be delivered even earlier than that.
Will, a lawyer, began his nearly hour and a half drive from court in Onslow County while Cleere was admitted to the hospital for more ultrasounds and tests.

“Basically they figured out that they didn’t think it was safe for the baby to be in the womb anymore,” Will said. “And then the question was, well how long can he be in there?”
Sledge Strong

Photo courtesy of Reaves family
The time frame changed quickly as the team at Maynard Children’s Hospital reviewed the situation. Among several other factors, the ultrasound revealed that there was fluid around Sledge’s liver and near his brain, prompting doctors to be extremely concerned about a serious condition called hydrops, which can be life-threatening for premature babies.
Cleere was taken back about 2 p.m. that same day, July 23, to deliver her baby boy. As William Sledge Reaves was born, doctors could tell right away there was no sign of hydrops – the first big win in the life of a young fighter.
“It was really incredible because I can definitely tell you, there were angels in that room that helped him,” Cleere said. “I have no doubt that the Lord was very much present in that room and fighting for him.”
Sledge, with an appropriately tough name, weighed just 1 pound, 12 ounces at birth and was intubated right away to help him breathe. Intubating a child so small was another early win.
Sledge has been in the Neonatal Intensive Care Unit (NICU) at the Maynard Children’s Hospital since his birth and continues to get stronger and face the ups and downs of his young life.
Life in the NICU

Cleere and Will said they often hear the term “NICU rollercoaster ride” as they navigate this time with their newborn son. There are plenty of wins and challenging times, but Will and Cleere both said the support of team members in the NICU keep them on track.
“The providers are really helpful with that,” Will said. “If Sledge does have a tough day with one thing, they’ll say look at all these other great things that happened today. It’s hard but it’s a great reminder.”
“You’re kind of trying to coach your mind to say ‘Hey, this is part of the ride and sometimes what feels like a back step is not. His body is learning, all his systems are growing, he’s maturing and this is part of it,'” Cleere said. “It’s really just having such a sense of trust that they’re good at what they do, this is not their first rodeo, so Will can be the dad and I can be the mom – because that’s what Sledge needs and he can feel that from us I think.”
Trusting the care team is an invaluable part of life in the NICU, Will and Cleere agreed. They said it’s not natural to have a baby and leave the hospital to go home with their child staying behind.
The camaraderie with the care team and welcoming team members at every turn who care for physical and emotional needs make it easier to sleep at night and come back into the Maynard Children’s Hospital each day to spend time with their baby boy and focus on being parents.
“I think it starts when you walk into the Children’s Hospital,” Will said. “Whether it’s Jackie, Barbra, Lee or anyone out there at the front desk who are just inviting and welcoming and asking how Sledge is doing. It starts there and then continues to when you get back and see Mr. Lawrence, Natasha or MJ and they’re asking how he’s doing, how you’re doing and making sure you have everything you need.
“Then, his primary care nurses, nurse practitioners, doctors – there are too many to name, there’s so many of them – they just make you feel like ‘Hey, we’re all here, we’re all in this together.’ That’s amazing when you consider the fact that every single one of them has been working 12-hour shifts. Whether you walk in at 7 a.m. or 7 p.m., you’re getting the same positive attitude.”
Moving Forward
 Cleere and Will said Sledge still has a long road ahead of him and they are proud of their son for all he has overcome to this point. Cleere has a mantra that she heard early on in their experience and keeps close to her heart through their time in the NICU.
Cleere and Will said Sledge still has a long road ahead of him and they are proud of their son for all he has overcome to this point. Cleere has a mantra that she heard early on in their experience and keeps close to her heart through their time in the NICU.
“As a mom, you just pray that he rests and grows and I think about that all the time,” Cleere said. “He’s going to have his bumps, we’ve had them and we’ll still have some. Then we’ll have it where we coast a little bit. But as he rests and as he grows, he’ll be able to handle and fight whatever comes his way and he’ll move right along.”
Sledge has come off of his ventilator but still receives some respiratory support. His feedings are growing and so is he as he was up to 4 pounds, 6 ounces at nine weeks.
The Reaves family looks forward to everyone being home together, but until then Sledge will continue to live up to his tough name and fight with parents and a care team by his side.
Greenville, N.C. – Sept. 28, 2021 – Since 1989, The North Carolina Great 100, Inc. has recognized and honored nurses around the state for their commitment to excellence and to promote a positive image of the nursing profession. Out of thousands of nominations that are submitted annually, 100 recipients are selected based on their outstanding professional abilities and contributions made to improving health care services to their communities.
This year, 14 ECU Health Medical Center (VMC) nurses have been selected to the 2021 NC Great 100.
Vidant Health extends heartfelt gratitude to these nurses for their contributions to patient care and living the Vidant mission of improving the health and well-being of eastern North Carolina.
The Vidant nurses chosen this year are:
Anthony Ayscue, BSN, RN, CRN, is the assistant nurse manager for ARU, VAT and Radiology Nursing at VMC. Anthony has been with Vidant for more than 18 years and has been in his current role for more than five years. Anthony is a certified radiology nurse, and earned an associate’s degree from Edgecombe Community College and a bachelor’s degree from Barton College. He is a member of the Association for Radiologic & Imaging Nursing.

Youssef Belahchich, RN, is a staff nurse III working in the Neurosciences Unit at VMC. Youssef has worked at Vidant for seven years and previously served as an orthopedic RN. He graduated from Pitt Community College with an associate degree in nursing and worked in a skilled nursing facility before joining VMC.

Amy Campbell, PhD, RN, CPHQ, LSBB, is a quality nurse specialist III on the Performance Improvement Quality Analytics team at VMC. Amy started her career as a staff nurse on the pediatric floor at the former Pitt Memorial Hospital in 2000. Amy has been in her current role for 12 years. Amy earned an associate degree in nursing from Pitt Community College, bachelor’s degree in science nursing from East Carolina University (ECU), as well as a master’s degree and PhD in nursing from ECU. She is certified in Lean Six Sigma Black Belt from North Carolina State University and is a certified professional in Health Care Quality. Amy was an East Carolina Hall of Fame doctoral scholar and the 2018 Association for Leadership Science in Nursing Doctoral Grant recipient. Amy is a member of National Association of Healthcare Quality, Association of Leadership Science and Sigma Theta Thau.
Michelle Carawon, MSN, RN, CCRN-K, is an infection control preventionist III at VMC. Michelle has been with Vidant for 16 years and has been in her current role for the past year. Michelle is certified in critical care nursing and earned a bachelor’s degree in nursing from East Carolina University and a master’s degree in nursing from Walden University. Michelle is a member of the American Association of Critical Care Nurses, Sigma Theta Tau-International Honor Society of Nursing, the Association for Professionals in Infection Control and the East Carolina University Alumni Association.

Miriam Coggins, BSN, RNC, is a staff nurse at VMC’s Neonatal Intensive Care Unit (NICU). Miriam has worked in the NICU at VMC for 36 years. She earned a bachelor’s degree in science nursing from East Carolina University. Miriam has held multiple roles at VMC including permanent charge nurse, assistant nurse manager and interim manager. As interim manager she assisted with the opening of VMC’s current 50 bed NICU. Miriam has a certification in neonatal intensive care and serves as co-chair of the Central Line Team.

Roland Ennis, RN, is an assistant nurse manager of the Orthopedic Unit at VMC. Roland has been with Vidant for 21 years and has served in his current role as assistant nurse manger for 10 years. He earned an associate’s degree in nursing from Edgecombe Community College.

Amanda Helms, BSN, RN, is a staff nurse III in the Trauma Surgery Intermediate Unit at VMC. She has been at Vidant for 15 years and has served in her current role for nine years. Amanda earned an associate’s degree in nursing at Beaufort County Community College and received a bachelor’s degree in nursing from University of North Carolina at Wilmington. Amanda obtained trauma nursing core course certification and is a member of the American Nurses Association, North Carolina Nurses Association, Society of Trauma Nurses and Sigma Theta Tau International Honor Society of Nursing.

Kristie Hertel, MSN, RN, CCRN, ACNP-BC, FCCM, is an advance practice provider with the Trauma and Surgical Critical Care Department at VMC. Kristie started at VMC in 2006. Kristie earned a bachelor’s degree from Nazareth College, a master’s degree from Rush University and is currently enrolled at UNC Wilmington working toward a doctorate in nursing practice. She has received specialty certification as a certified critical care nurse and acute care nurse practitioner along with induction as a fellow in the Academy of Critical Care Medicine. Kristie is a member a member of the American Association of Critical Care Nurses, Society of Critical Care Medicine and Sigma Theta Tau International.

Stephanie Head, MSN, RN, PMGT-BC, NE-BC, is the nurse manager of the Vidant Pain Management Center, a hospital outpatient department of VMC. A Vidant nurse for 30 years, Stephanie has been the manager at the Vidant Pain Center for the past nine years. Prior to her current role, Stephanie served as a nursing assistant for two years. Stephanie earned a bachelor’s degree and master’s degree in nursing leadership from East Carolina University. She holds a specialty certification in pain management nursing and is a nurse executive-BC. Stephanie is an active member with American Society of Pain Management Nurses and North Carolina Organization of Nurse Leaders.
Patty Jordan, MSN, RN, NE-BC, CCCC, is a senior nurse administrator in Patient Care Services at VMC. Patty has been with Vidant for five years. She earned a bachelor’s of science degree in nursing and a master’s of science degree in nursing and health care administration from Southern Illinois University – Edwardsville. Patty has obtained specialty certifications as a nurse executive, and as a cardiovascular care coordinator. Patty is a member of American Association of Critical Care Nurses, East Carolina Chapter of American Association of Critical Care Nurses, American Organization of Nurse Leaders, Sigma Theta Tau, and the North Carolina Nurses Association.

April Meeks, BSN, RN, PCCN, is the assistant nurse manager on the Palliative Care Unit at VMC. April has been with Vidant for 15 years and in her current role for more than a year. She earned an associate degree in nursing from Edgecombe Community College and a bachelor’s degree in nursing from the University of North Carolina at Wilmington. April is specialty certified as a progressive care certified nurse. April is a Daisy Award Honoree and a Vidant Brody Award Finalist. April is a member of the American Association of Critical Care Nurses, North Carolina Organization of Nurse Leaders, North Carolina Association of Healthcare Quality and Sigma Theta Tau.

Shannon Mazza Roberson, BSN, RN, CPEN, SANE-P, is a staff nurse IV in the Special Care Nursery at Maynard Children’s Hospital. Shannon has been with VMC for the past eight years and she earned a bachelor’s degree from Barton College. She began her career with Vidant in the Children’s Emergency Department as a staff nurse. Shannon has been a part of the leadership team within Emergency Services as both assistant nurse manager of the Children’s ED and nurse manager of the Adult ED. Shannon has more than 23 years of nursing experience and has cared for pediatric patients throughout her career. She is a certified pediatric emergency nurse as well a sexual assault nurse examiner for pediatrics. She is a 2020 finalist for the Vidant Brody Award as well as a Daisy and Team Daisy Award recipient. Shannon holds multiple certifications in the field of Emergency Services. Shannon is a member of the International Association of Forensic Nurses, the Emergency Nurses Association and a member of Sigma Theta Tau.

Sherry Stone, DNP, RN, NPD-BC, is an education specialist in nursing at VMC. Sherry has been at Vidant for six years. She earned an associate degree from Patrick Henry Community College, a bachelor’s degree from Old Dominion University, a master’s degree from Western Governor’s University and a doctorate in educational leadership from American Sentinel University. Sherry has obtained certification in nursing professional development. She is a member of the American Nurses Association, the North Carolina Nurses Association, the National League for Nursing and The Association for Nursing Professional Development for which she serves as the chair for the Recognition Committee.

Ashley Venters, MSN, RNC-LRN, is a staff nurse III in Special Care Nursery at VMC. Ashley has been in her role for more than 14 years and earned a bachelor’s degree and master’s degree in nursing education at East Carolina University. Ashley is currently working towards post-master’s work in the field of family nurse practitioner. Ashley obtained her specialty certification in low-risk neonatal nursing and is a member of Beta Nu and Sigma Theta Tau.
Greenville, N.C. – June 28, 2021 – The 2021 Vidant Health Board Quality Leadership Award winners were recently recognized by the Vidant Health Board of Directors for their improvement of patient care. These winning teams are a representation of excellent work across the system that drives the quality goal of zero harm, creates exceptional experiences and improves patient outcomes. Nine nominations were reviewed by the committee and the winning teams are as follows:

- Vidant Edgecombe Hospital: “Impact of a Palliative Care Program in a Community Hospital” was selected for its work in reducing the mortality rate and readmission rate by five percent.
- Vidant Family Medicine – Edenton: “Responding to COVID-19: Building an Airplane While Flying” for its work to establish a fully functioning respiratory clinic by April 9, 2020, that would see patients requiring screening, testing and treatment for COVID-19 infections.
- ECU Health Medical Center, Maynard Children’s Hospital team: “A Sustained Improvement in CLASBI Reduction” for its work to reduce central line associated blood infections in Maynard Children’s Hospital by 50 percent.
To receive this honor, team members submitted projects that demonstrated at least two of the following requirements:
- Quantifiable improvement in an organizational quality priority with sustained excellence over time
- Demonstration of empathy and compassion in patient care
- Implementation of innovative solution to patient care problem
- Community outreach that addresses the social determinants of health in a meaningful way
“We are proud to see team members from across Vidant Health recognized for their hard work and dedication to patient care,” said Dr. Shirley Carraway, Ed. D, chair of the Vidant Health Board of Directors. “The pandemic brought unique challenges to healthcare and these team members continued to innovate and improve the health and well-being of eastern North Carolina, and we are proud to honor them in this way.”
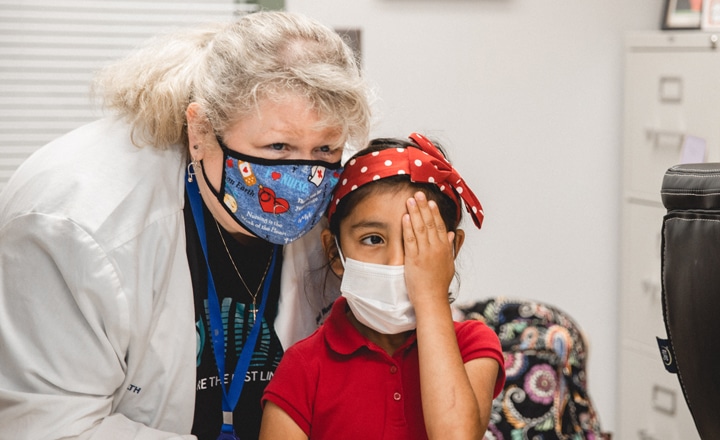
“May 12 is National School Nurse Day, so there is no better time to celebrate the incredible work that our school nurses do in Pitt County Schools,” said Catherine Nelson, senior administrator of community health at VMC, and a founding member of the School Health Program. “They have helped us safely mitigate the spread of COVID-19 while getting our students back in school for in-person learning, and continued to excel in their daily case management among students.”
Vidant launched the program in partnership with the ECU College of Nursing, Pitt County Public Health and Pitt County Schools in 1996. The program has grown from six registered nurses at 19 elementary schools to 21 nurses at 39 schools. The School Health Program was recognized by VMC in March 2021 for having the most certified nurses in an ambulatory care setting. School nurses complete daily tasks from overseeing the administration of medications to performing life-saving measures.
“At Pitt County Schools we value our partnership with Vidant and consider ourselves fortunate to have the terrific team of nurses to serve our students throughout these past 25 years,” said Karen Harrington, Director of Student Services. “The demands on school nurses continue to increase annually but never before have we been challenged to this level. This year, our nurses never stopped working – even when the rest of the system was in quarantine – and their efforts and time this year have not gone unnoticed. Not only have our nurses supported student health but they are a valuable resource to our staff. Please take time to thank a school nurse this week. And thank you to Vidant for your continued partnership.”
“The school nurses have been instrumental in getting their school staff trained and prepared for the use of Stop the Bleed kits,” Erika Greene, pediatric trauma program manager for Maynard Children’s Hospital at ECU Health Medical Center, said. “We have expanded our outreach to Wayne County Schools while working towards our goal of providing education and placement of Stop the Bleed kits at each public school within the 29-county Vidant Health region.”
One of the most common contributing factors in trauma-related events is preventable blood loss. Approximately 40 percent of trauma-related deaths worldwide can be attributed to bleeding or its consequence. The items in these kits help control the loss of blood, leading to positive outcomes for those who sustain injuries.
The Stop the Bleed Kits are funded by Children’s Miracle Network along with training in the use of a combat tourniquet provided by Maynard Children’s Hospital. They were distributed to Wayne County Schools with education to ensure schools are prepared in the event of a trauma incident.
The Pediatric Trauma Department of Maynard Children’s Hospital distributed 66 kits to cover the 33 public schools in Wayne County with the assistance of the VMC Trauma Outreach Coordinator.
“Vidant Health provided an awesome comprehensive Stop the Bleed training for the school nurses of Wayne County Public Schools,” said Kim Kennedy, manager of School Health Services for Wayne County Schools. “Thanks to Stop the Bleed and The Children’s Miracle Network, all WCPS campuses will be equipped with tourniquet kits that can be utilized in the event someone suffers severe bleeding. We thank Vidant Health and The Children’s Miracle Network for sponsoring this vitally important project.”
Pediatric neurosurgery is the surgical treatment of diseases of the brain and spine in children. This includes a wide variety of conditions, from ones that children are born with, to others that children acquire later in life.
Dr. Kathleen Knudson, a pediatric neurosurgeon with Vidant Neurosurgery, shares her experiences and her process for working with patients and their families.
“When I am trying to decide on the best plan for the patient, I look at the entire person,” she said. “I talk to them and find out what they are concerned about and get a detailed neurological exam. I often get an imaging study, depending on what their concern is. Then, I use all this information together, (the history, exam, and imaging) to make a recommendation on surgery. I don’t just look at the imaging alone to make a recommendation.”
In this process, Dr. Knudson works together with the patient and their families to come up with the right treatment for the child.
“It is a team effort,” she said. “I work closely with other Vidant team members, including pediatric oncologists, pediatric neurologists, general surgeons, pediatric orthopedic surgeons, and many other providers to help take care of the patient.”
Dr. Knudson added, “Often, there is more than one surgical option for patients. I go over these different options with the family to decide what is the best plan for everyone. I often recommend minimally invasive surgery, so the child will have a smaller incision and a faster recovery.”
Pediatric neurosurgery patients are seen and treated at the Maynard Children’s Hospital in Greenville. If your child may require neurosurgery, talk to your provider for a referral to Vidant Neurosurgery. If you do not have a Primary Care Provider, Vidant Health can help you find one by calling 1-800-472-8500. You can also learn more on the Neurological Care page.
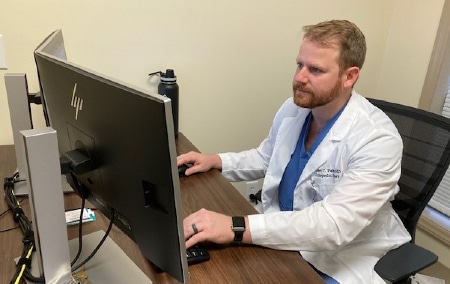
“Being a pediatric orthopedic surgeon is unique because we are responsible for treating the whole child,” Dr. Palmer said. “We see so many unique cases, from limb deficiencies, to physical deformities and traumatic injuries like broken bones. This means the relationship I build with my patients and their family is not centered around a single surgical event, but rather the unique treatment and healing process catered to help that child get back to life.”
Pediatric orthopedists specialize in treating bone, joint or muscle problems and the care continuum using both surgical and nonoperative treatment modalities for pediatric patients depending on the severity of their condition. Cases range from physical conditions from birth to sports-related injuries. Using innovative rehabilitation strategies, the goal is to safely and expediently get the patient back to his or her baseline level of function.
Patients and families can expect a coordinated process that usually involves the primary pediatrician, orthopedic surgeon, physical therapist and sometimes even the child life specialists at the Vidant Health Maynard Children’s Hospital at ECU Health Medical Center, who specialize in supporting pediatric patients throughout the healing journey.
“One of the most important aspects of treating pediatric patients is being able to clearly communicate,” Dr. Palmer said. “There is a lot of fear that can come with a patient, especially the younger ones that may not understand their condition or injury. I have a young daughter myself and my approach is to treat the patient and family as if I was in their shoes.”
With resources across Vidant’s 29-county service area, the healing process post-surgery is designed to keep care as close to home as possible, reducing the need for long car rides which can be a hindrance for children in pain.
“This is the best job in the world,” Dr. Palmer said. “I get to help a child and their parents through one of their most difficult times. It is an amazing feeling and I am incredibly grateful to have that opportunity.” For more information about pediatric orthopedics, please call Vidant Orthopedics-Greenville at 252-816-4001.
Read more in The Daily Reflector
To celebrate World Kindness Day, Vidant Health and the Eastern Carolina Injury Prevention Program (ECIPP) at Maynard’s Children Hospital at ECU Health Medical Center would like to recognize the students in the Pitt County Students Against Destructive Decision (SADD) program for their work bringing kindness and education to area schools.
Since its inception in 2016, Pitt County SADD has positively impacted more than 25,000 students, parents, and community members through school club meetings and events, community-based initiatives and social media interactions. Students have presented on destructive decisions at local and state conferences and been recognized on countless local, state and national platforms for their work promoting positive decision making in Pitt County.
While there have been obvious activities such as Kindness Campaigns, leaving sticky notes with positive messages and the painting of a rock with the motto “Be Kind. Be Strong. Be Smart.”, every activity, event,or engagement coordinated through Pitt County SADD carries the same overarching message of just “Be Kind”.
A highlight of SADD’s 2020 campaign for kindness included a brand new website, PittCountySadd.com, designed by The Oakwood School student and SADD Student Leader Ellie Osborne. The website currently covers five main content areas: Mental Health, Road Safety, Know Your Ws, Vaping, and Social Media Safety.
“As a part of my Girl Scout Gold Award, I created a website for all of Pitt County SADD,” Osborne said. “I am so excited and grateful that the website has officially launched, and hope that it remains a great resource for youth of all ages regarding physical and mental well-being and support.”
Pitt County SADD is funded by Children’s Miracle Network, Vidant Health Foundation, Pitt County ABC Board, and Pitt County Schools, and is in partnership with the Safe Communities Coalition and ECIPP. Pitt County SADD is a peer-led program that empowers young people to successfully confront the risks and pressures that challenge them throughout their daily lives. The mission is accomplished by creating, equipping, sustaining a network of student-run chapters in schools and communities.
“It is student leaders like Ellie and our countless other SADD members that have been the driving force behind some of our strongest prevention efforts,” Sue Anne Pilgreen, program manager for ECIPP, said. “As a leader in children’s health care for eastern North Carolina, the partnership that we have with the schools and community is crucial and these students are making a positive impact on making the world more kind.”
One of the most common contributing factors in trauma-related events is preventable blood loss. Approximately 40% of trauma-related deaths worldwide can be attributed to bleeding or its consequence. The items in these kits help control the loss of blood, leading to positive outcomes for those who sustain injuries.
The Stop The Bleed Kits are funded by Children’s Miracle Network with training provided by Maynard Children’s Hospital. They are distributed to all Martin, Greene and Pitt County Schools with education to ensure schools are prepared in the event of a trauma that results in active bleeding that could endanger a child’s life. These kits will ensure that more children can be treated and with supplies that last long-term without expiration.
“The school nurses have been instrumental in getting their school staff trained and prepared for the use of Stop The Bleed kits,” Erika Greene, pediatric trauma program manager for Maynard Children’s Hospital at ECU Health Medical Center, said. “In total, more than 100 kits have gone to the schools in Greene, Martin and Pitt Counties. It is our hope that over the next few years, we will provide education and place Stop The Bleed kits at each public school within the 29-county Vidant Health region.”
Dr. Ethan Lenker, Superintendent, Pitt County Schools, added: “Thank you, Vidant, for pushing this training out to many organizations and businesses in the community, including our school system. Because of this great partnership, many PCS staff members are trained in Stop The Bleed techniques including our First Responders and many of our administrators. We are also grateful to be a recipient of the kits as vital, lifesaving equipment in our schools.”