The American Association of Cardiovascular and Pulmonary Rehabilitation’s (AACVPR) Day on the Hill, which was March 4-5 this year, is an opportunity for cardiac and pulmonary rehabilitation professionals to visit Washington, D.C. to advocate for their profession and ask legislators for support for beneficial legislation on Medicare decisions. It was Stacey Greenway’s 10th year participating in this event, a milestone made all the more significant by her recent election as treasurer to the AACVPR board.
Stacey, the director of cardiovascular disease management services at ECU Health Medical Center, wasn’t initially interested in health care policy, but her zeal for her work inspired her to get involved.
“I’m passionate about what I do, and when I realized the impact these legislative decisions make on our patients, I wanted to get involved,” she said. “When the North Carolina Cardiopulmonary Rehabilitation Association (NCCRA), which works on the state level, asked if anyone was interested in participating in Day on the Hill, I thought how cool it would be to help our patients and our programs. After the first time, I was hooked.”

Each year, the AACVPR’s legislative priorities are different, but the goal is the same. “We want to help the legislators see things from the patient perspective and put a face to the people these bills are affecting,” Stacey said. “From that angle, you see the increase in a patient’s quality of life. From a health system perspective, it decreases the rates of hospital readmission. It’s a win-win.”
This year’s priorities centered on two bills: HR-955/S.1849, the Sustaining Outpatient Services Act, and HR-1406/S.3021, the Sustainable Cardiopulmonary Rehabilitation Services in the Home Act. The Sustaining Outpatient Services Act seeks to correct a legislative error from a previous bill that reduces reimbursement for cardiac and pulmonary rehabilitation services when they are provided in off-hospital campus clinics. The reduced reimbursement rate makes cardiac and pulmonary rehabilitation services financially unsustainable and thus eliminates patient access to these resources, especially in rural communities. “Some rural hospitals, which don’t have a lot of real estate on campus, haven’t even tried to open a rehab clinic because of this issue,” Stacey said. This bill would establish an exemption status to certain hospital outpatient services, including cardiac and pulmonary rehabilitation, from that fee reduction.
The Sustainable Cardiopulmonary Rehabilitation Services in the Home Act would allow Medicare beneficiaries to receive cardiac or pulmonary rehabilitation services through real-time telehealth in their homes. This hybrid type of service was very successful during the pandemic, and it allowed more patients to be treated from across eastern North Carolina.
“Think of that 45-year-old patient who had a heart attack and would benefit from rehab services but has also been cleared to work and needs to make an income,” Stacey explained. “This bill would allow that patient to not have to make a choice between income and health; they could do both.”
During her time in Washington, D.C., Stacey and 74 other AACVPR members spoke with their respective House Representatives and Senators to advocate for these bills. Stacey said overall, the discussions were productive.
“I had some good conversations about both bills,” she said. “The telehealth bill was one the legislators could wrap their heads around easier; it was something they were familiar with. That was encouraging.” While more work needs to be done to increase support for the outpatient services bill, Stacey said she felt the needle moved a bit. “This is partly because the government seems to be changing their focus from thinking about the up-front costs of health care to the savings incurred on the back end,” Stacey said. “That means things are changing, and I’m hoping we’ll get a few more co-signatures on that bill.”
As a board member, Stacey said she now has other opportunities to support her profession.
“To represent eastern North Carolina and discuss at the national level some of the things that impact those who practice locally is really important,” she said. Because she was on the board this year, Stacey was also able join the board meeting the day before Day on the Hill and participate in the selection of a new legislative firm. “We met with the firm and prepped for Day on the Hill, but we also strategically planned for the future,” Stacey said. “It was exciting to be involved in that process.”
Stacey’s interest in running for the AACVPR’s treasurer position stemmed from her desire to stay involved in the national organization and escalating care for patients.
“The board is involved in regulatory and government relations, and that’s one of my big interests. Day on the Hill is just one way we stay involved. It’s a way of understanding and supporting initiatives and bringing that back to ECU Health,” she said. “We have six cardiac and pulmonary rehab programs within ECU Health, and I want to make sure those programs are aware of the initiatives the AACVPR promotes to escalate their practice and ensure we’re doing the best we can for our patients.”
Now that the initial conversations with Congress members are over, the next step is to follow up in a few weeks with those representatives still on the fence. “We’ll also bring in a constituent from that person’s district to speak to the impact of these bills,” Stacey said. Some representatives have already signed on to at least one of the bills, including Rep. Don Davis, Rep. Deborah Ross, Rep. Greg Murphy, Rep. Wiley Nickel and Rep. Jeff Jackson.

It’s important to be involved in the policy issues surrounding health care, Stacey said. “You don’t go into health care thinking about these operational or political issues, but when you’re faced with the repercussions in the clinic, you see the impact it has.”
She encouraged all health care professionals to get involved: “Let’s do this for the betterment of the patient experience,” she said. “For me, this has been one of the highlights of my professional life.”
As part of its commitment to growing a high-quality nursing workforce for the region, ECU Health recently held a New Graduate Nurse Hiring event to connect with upcoming nurses, many of whom will begin their career with the organization in a few months.
The two-day event was hosted at the TowneBank Tower and the Williams-Clark Club Level on East Carolina University’s campus.
The February hiring event featured 301 scheduled interviews with prospective nurses, many of whom are from right here in eastern North Carolina, allowing candidates to interview for various units and connect with nursing leaders within the organization. To date, 96 future nurses have accepted positions across the ECU Health system.
This event underscores ECU Health’s commitment to recruiting and retaining exceptional nurses as we continue to shape the future of rural health care.

“The New Graduate Nurse Hiring event was really a great turnout,” said Trish Baise, chief nursing executive, ECU Health. “The opportunity to connect with future nurses was priceless. It was beneficial to engage in a casual environment before interview day and it allowed our team to speak with them informally. Every year it gets better. New graduate nurses are an important part of our workforce pipeline. It’s important for us to make sure that those who have grown up in eastern North Carolina and/or have been educated here, have a wonderful clinical experience with us.”
The hiring event spanned two days, with Friday dedicated to networking and allowing candidates to interact with recruiters and nursing leaders from several ECU Health entities, and Saturday dedicated to interviews.
“The key message that resonated well with the nursing candidates was ECU Health is the land of opportunities,” said Dr. Kamilah Williams, administrator for Professional Practice Development & Clinical Education at ECU Health. “There are so many opportunities for launching nurses’ careers in every specialty of nursing practice across ECU Health.”
If you’re interested in reading about our new graduates and their experience at ECU Health, check out the People of ECU Health articles on Brianna Cavaliere and Samantha Nichols.
“Jim will be very humble and tell you he was in the right place at the right time,” Dr. April Quidley, pharmacy supervisor, critical care/emergency medicine and PGY1 Pharmacy Residency Program director, said about Dr. Jim Worden’s impact on ECU Health and in his community.
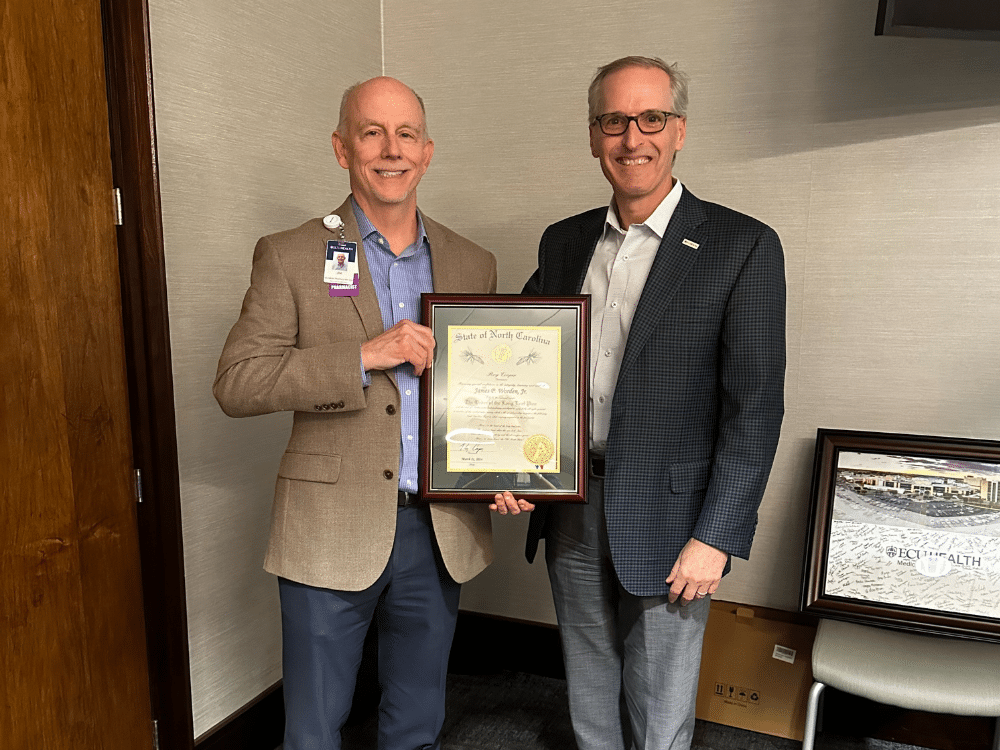
Dr. Worden retired on March 22 after working for ECU Health for 41 years. During his retirement reception, however, he was surprised to learn he’d also won the Order of the Long Leaf Pine award, the highest honor North Carolina’s Governor can bestow on a person for their contributions to the state.
Dr. Worden, a Tennessee native, moved to Greenville, North Carolina for his first job out of his pharmacy residency to work as a clinical coordinator. “I’ve been here [at ECU Health] since August of 1983,” Dr. Worden said. During that time, he held a few different roles, including assistant director of clinical services, the director of pharmacy and most recently, the systems service line administrator for pharmacy.
During that time, Dr. Worden was instrumental in setting up ECU Health’s pharmacy services by “working closely with physicians in a direct, bedside patient care role” and by founding the Drug Information Center, which, according to Dr. Worden’s award nomination documents, “served as a resource for all health disciplines in eastern North Carolina in the time that evidence-based medical practice expanded.”
“When we think about pharmacy services at ECU Health, Jim is the guy who gets all the credit,” Dr. Quidley said. “He worked hard to form those interdisciplinary relationships with physicians and to advocate for patients. He is the founding director of our residency program, the Pharmacy Practice Residency, which is one of the oldest in the country at 30 years old.”
He went on to develop additional pharmacy residency training programs for critical care, emergency medicine and infectious diseases. “He’s been on the cutting edge of everything we do in pharmacy,” Dr. Quidley said. “He’s done exceptional things for the department.”
As a result of his dedication, ECU Health’s services represent a leading practice in pharmacy care, especially for a rural region, and he’s helped expand services to improve the medical and pharmacy care across all of eastern North Carolina.
On March 22, a retirement reception was held to celebrate Dr. Worden’s more than four decades of service. Little did he know, however, that there was an ulterior motive to the event. “We surprised him with the Long Leaf Pine award at the event,” Dr. Quidley said. “Dr. Mike Waldrum, Dr. Herb Garrison – also a recipient of the award – and Brian Floyd were there to present the award to Jim, and it was a great surprise.”
The Order of the Long Leaf Pine award is among the most prestigious awards conferred by the Governor of North Carolina, and it is awarded to persons for exemplary service to the state and their communities, going above and beyond the call of duty and making a significant impact on and strengthened North Carolina. Nominations can be made for retiring individuals who have 30 or more years of service in North Carolina, and nominations must include documents that attest to the person’s work and service, supported further by letters of recommendation.
Dr. Worden said he knew of the award, but he didn’t think he was the sort of person to win it. “It’s an impressive, austere award, but I didn’t think I’d done anything in my life that was at the level to win it. I was humbled to be considered for something that noble.”
Dr. Quidley and those who wrote supporting letters of recommendation think differently. Dr. Worden has made a significant impact not only at ECU Health, but also in his community. He is on the Board of Directors for the Community Crossroads Center, which is the only emergency homeless shelter in Greenville and Pitt County. He joined the board three years ago after a fellow church member let him know a position was opening.
“I felt like my conscience told me I should apply, that God was calling me to help, so I applied, and they voted me in,” Dr. Worden said.
In the past year, he worked with ECU Brody School of Medicine to restore medical services for residents of the shelter. For his dedication to the board and the shelter, the board elected Dr. Worden to be president next year. He is also actively engaged in Greenville’s First Presbyterian Church, where he has in the past served as the Chair of the Missions Ministry, Chair of the Worship Ministry, a member of the Stewardship committee and twice as an elder on the Session, the church’s governing body.
“I’m very committed to my church,” Dr. Worden said. He plans to continue that service now that he’s retired. “I’m going to enjoy time away from work, but I won’t be sitting around. I will of course be the president of the shelter’s board, and we will have activities that will keep me busy. I will continue to work in my church, and I hope to play some tennis and pickleball.”

Dr. Worden also plans to travel with his wife of 34 years, Tammy, who is also a pharmacist at ECU Health and who helped Dr. Quidley nominate Dr. Worden for the Long Leaf Pine award. “When you’ve been married to someone that long, it is an accomplishment – you need that person and they need you,” he said.
As Dr. Quidley predicted, Dr. Worden remained humble about his contributions to ECU Health and beyond.
“This is not about me,” Dr. Worden said of winning the award. “I’ve started some good things, and I’ve been fortunate to have the resources, teamwork and leadership to do these things, but it really does take a village. I will take credit for some of it, but a leader can only do so much by themselves.”
Tanya Graham, a North Carolina native and Greenville resident, was outside cutting her grass when she started to feel very tired. That night, she experienced what felt like an asthma attack, so the next day she visited an urgent care clinic. “I do have asthma,” Graham shared, “but I’ve never had an attack.” The doctor ran a few more tests, and after an EKG, he decided to send Graham to the hospital.
“The cardiologist at [ECU Health] Medical Center said, ‘You are in heart failure,'” Graham said. “I didn’t know what he was saying, I was so shocked.”
Dr. W. Douglas Boyd, a cardiothoracic surgeon, told Graham she needed surgery, and two weeks later, Graham found herself back in the hospital recovering from a double coronary bypass. She was told later that her initial ejection fraction, which is the amount of blood your heart pumps each time it beats, had been 10 percent. A normal ejection fraction is 50 percent or higher. “After the surgery, they did another echocardiogram, and now it’s up to 35 percent,” Graham said.

Graham knew that once she was strong enough after the surgery, she wanted to participate in cardiac rehabilitation. She had heard about the option from her neighbor, who also had recently suffered a heart attack. “I also have two sisters who are nurses,” Graham shared. “One of them works for a cardiologist, so I talked with her about cardiac rehab, and all of my siblings agreed it was a good idea.”
Cardiac rehabilitation focuses on the “what now” after a cardiac event. Stacey Greenway, the director for cardiovascular disease management services at the Medical Center, hopes that cardiac rehab will become the immediate program associated with cardiac recovery.
“A multidisciplinary team works with the patients to establish and achieve goals to improve their health, quality of life and functional ability,” Greenway said. “We develop individualized treatment plans for each patient that includes exercise, nutrition, medications, stress management and other components.”
For Graham, therapy started slow, but she said she immediately felt comfortable. “The team is so smart, and they are in tune with each individual person,” Graham said. “It made a huge difference because I learned right off that I could trust them. It made me want to go.”
It also helped to have others around her going through the same experience. “It didn’t matter if they were a man or woman or what race they were – we were all there for the same reason. Our bodies had broken in some way, and we were all there together for the same purpose of trying to survive and extend our lives,” Graham said. “I drew strength from them, because when I saw them working hard, it made me want to do the same.”
The experience didn’t just provide Graham with the chance to get stronger after a major surgery. “The one thing I came away with,” Graham said, “is hope. Hope that I’d live a longer life.” Graham said that it wasn’t just the exercise that encouraged her and helped her get better; it was also the classes they offered. “I learned quite a bit from the classes, which covered things like diet and coping with this diagnosis,” she said. Something Graham didn’t expect was having access to support from a therapist. “I’d had a hard experience with my surgery, so they put me in contact with Dr. Kari Kirian, and she worked wonders. I can’t say enough positive things about that experience.” Dr. Kirian is a cardiac psychologist embedded in the heart failure program – a critical member of the care team as it is not uncommon for patients to experience anxiety or depression after a cardiac event.
While she wished she could have participated for longer, Graham graduated from cardiac rehab with the ability to do the things she needs to do. “It allowed me to come home and do the things you take for granted, like clean the house or roll your hair,” Graham said. She also immediately joined a gym and signed up for personal training to continue her progress. “I left cardiac rehab on a Friday, and that following Monday I was at the gym,” Graham said. “It wasn’t mandated, but the cardiac rehab team provided me with information. My sister goes to a gym, so I decided to go there, and now I go every weekday. I will continue to exercise, think positive and eat right.”
Because she’s feeling so much better, Graham said she has plans for the future. “I’m going to work on making one of my bedrooms a storage space, and in the spring, I plan to paint a shed in the back yard,” Graham said. She also hopes to visit her daughter and grandchildren in Phoenix, Arizona next winter. In the meantime, Graham said she’s cleared it with her doctors to serve as a volunteer in the cardiac rehab unit. It’s one way she can share her experience and give back to the amazing Cardiac Rehab team for impacting her life in an incredible way.
“I don’t care what I do. I just didn’t want to leave there,” Graham said. “I love people, and I thought maybe if I was around people going through what I went through, I could tell them my story and help them.”
The Eastern Carolina Injury Prevention Program (ECIPP) at ECU Health Medical Center partnered with volunteers from Greenville Police Department, ECU Health Police Department, Pitt County Sheriff’s Office, ECU Police Department, Pitt County Schools and nurses at ECU Health to fit 100 fourth and fifth graders at South Greenville Elementary School with bicycle helmets to encourage safe biking. Funding for the helmets was provided by Children’s Miracle Network and the North Carolina Department of Transportation.
“It is incredibly important for parents to ensure their children know how to safely ride their bikes including wearing a helmet, bright colors and reflectors, riding on the sidewalk or in the same direction as traffic and being aware of their surroundings,” said Ellen Walston, injury prevention coordinator, ECIPP, ECU Health. “Wearing a helmet is the best way to reduce head injuries, and we are incredibly grateful to our community partners including law enforcement officers and physical education teachers that are willing to teach bike safety to their students.”

According to Safe Kids, properly fitted helmets can reduce the risk of head injuries by at least 45 percent, yet less than half of children 14 and under usually wear a bike helmet. In 2020, there were 136,753 emergency department visits from children with bicycle-related injuries across the country. ECIPP aims to reduce the number of children harmed in eastern North Carolina and beyond by encouraging safe bicycling practices and ensuring local children have access to helmets. These partnerships not only facilitate the distribution of helmets but also enable law enforcement officers to engage directly with children, emphasizing the importance of wearing helmets and adhering to traffic regulations while biking.
“While ECIPP may provide the logistical and often the boots-on-the-ground operations, none of our work would be possible without the strong partnerships that we have with our schools, law enforcement and many others throughout the region,” said Sue Anne Pilgreen, manager, ECIPP, ECU Health.
Haley Behm was completing one of her first rotations in the Brody School of Medicine at East Carolina University at an outpatient clinic when Cleve Smith showed up for a routine check-up with his father, Emmett Smith. Cleve, a wheelchair user, has seen his fair share of medical students come through the clinic throughout his visits over the years but this was his first time working with Behm.
As a medical student with limited patient interactions, Behm was nervous about how she would connect with one of her first real patients, let alone her first patient with a disability. But when she met a lighthearted, humorous father-son duo in the patient room, she felt a little more at-ease.
“I was running through a depression and anxiety screening, and I got to a question where it asked ‘Have you ever been so restless you couldn’t sit still?’” Behm recalled. “I felt so bad even having to ask him that question.”
A question that Behm initially dreaded having to ask turned in to the start of a punchline for Cleve and Emmett, and it’s one they’ve practiced more than once.

“Haley has been really sweet, and I haven’t forgotten her since the first time we met,” said Cleve. “I could see that question really bothered her because I laughed and she didn’t immediately. So I wanted to assure her everything was fine.”
Added Emmett, “Through the years we have met many medical students at the clinic, and the one I remember is Haley. She had such a kind, caring demeanor. She really cared about Cleve’s feelings and what she could do to help him.”
Behm’s connection with the Smiths was just one of the powerful stories shared at ECU Health and Brody’s fifth annual Legacy Teachers Celebration on April 5. At the Legacy Teachers Celebration, third-year medical students share their experiences in the forms of short stories, poems or videos that honors patients who taught them valuable lessons – the type that can’t be learned in the classroom but can last a lifetime. The event also provides an opportunity for students to reunite with their Legacy Teachers and honor the special connection.
“The stories we hear at the Legacy Teachers Celebration are really emblematic of the types of experiences our students have here at the Brody School of Medicine and ECU Health,” said Dr. Jason Higginson, executive dean, Brody. “Medical students learn so much important information in the classroom and on clinical rotations, but sometimes the most impactful lessons they learn come from those they have the honor of caring for. It’s so gratifying to see our students reconnect with the patients who left a lasting impact on their journey toward becoming a physician.”
For Behm, her experience with the Cleve and Emmett gave her a different perspective on her role as a patient advocate, especially for patients with disabilities who may face difficulties accessing the care they need.
“Patients with disabilities have various accessibility needs, which may not be evident before a visit. It is important to be flexible and modify plans, exams and surroundings,” said Behm.
In total, 22 medical students shared their stories at the Legacy Teachers Celebration, which featured gift baskets, a photo station, lapel pins and remarks from ECU Health and Brody leaders – all designed to create a memorable experience for students and their legacy teachers.
Dr. Michael Waldrum, CEO of ECU Health and dean of Brody, provided remarks at the celebration along with Dr. Higginson. Like the students, they shared their deeply personal stories of important lessons they learned as students.
The speakers shared common themes around the importance of positive, trusting relationships between patients and care teams.

“The relationship between a physician and a patient is a sacred one,” said Dr. Waldrum. “Each patient we interact with provides us an opportunity to reflect on who we are and why we do what we do. For these medical students, who are driven by their passion to make a lasting difference in the lives of others, this event provides them with an opportunity to reflect on the legacy teacher that made a difference in their educational experience.”
While Cleve, Behm and Emmett were able to reunite at Legacy Teachers and share their story and learn of other stories, Behm expressed how important the Legacy Teachers Celebration is to reflect on the lessons learned from patients.
“The biggest part of Legacy Teachers is I have something to learn from all of my patients,” Behm said. “And some make the lessons easier than others.”
To be a health care provider is to answer a calling. For some, the journey to health care is a straight line; for others, the road is winding. This series features stories from ECU Health team members who took the winding road, but found the destination to be worth the effort.
Lacey Boldyrev, staff nurse II in the Pediatric Intensive Care Unit (PICU), has worked for ECU Health since 2020. “I started in the middle of COVID,” she said. “My last semester of nursing school was entirely online and we weren’t even allowed to go into the hospital for clinicals, so it was a challenge.” Prior to attending Coastal Carolina Community College for her RN degree, Boldyrev was a stay-at-home mom while her daughters were young, and once they went to school, she pursued her dream of being a teacher.
“I started school but didn’t finish my degree,” Boldyrev said. “I was a substitute teacher and a paraprofessional in Brooklyn, where we lived, for seven years.”
At that time, she and her family moved to North Carolina where she worked in a preschool at Camp LeJeune until the birth of her son.
“He was born at Onslow Memorial Hospital,” Boldyrev said. “We had a normal pregnancy and ultrasounds, nothing special. But after he was born and I went to get him, they told me I couldn’t pick him up. They told me to return to my room and the doctor would see me.”
It was at that moment Boldyrev learned that her son had congenital heart disease and the hospital was sending him to Maynard Children’s Hospital at ECU Health Medical Center in Greenville. “I had never had a child with health issues before,” Boldyrev said. “All of the sudden we’re living in a hospital for a year and a half and taking medical flights to different states.” Her son died on Christmas Day, 2015.
“After he was gone, there was this big empty hole,” Boldyrev shared. “I didn’t know what to do with myself.” The time she spent with her son in the hospital, she said, inspired her to pursue a degree in nursing. “I had given him his medications and his oxygen and feeding tubes,” she said. “All these things I’d done for him, and I learned from the nurses taking care of him. I took that as a sign.”
Although she had never previously considered a career in health care, her work with children in education set a foundation for how to communicate with kids and their families in the hospital. “I understood from my work in the schools some of the challenges children face and how they develop,” Boldyrev said.
After graduation, Boldyrev knew she wanted to work at Maynard Children’s Hospital. “Everyone who was working there when my son was there treated me with such compassion and listened to me. The PICU was the only place I wanted to be; I’m not sure I’d be as happy if I was anywhere else.”
Part of what makes her work so special, Boldyrev said, is the PICU team. “The reason I came back to Greenville, and keep in mind I commute over an hour to get here, is my team,” she said. “The people I work with provide exceptional care. Not once since I started have I felt alone or that my team doesn’t have my back. There are other places I could work that are closer but that’s not what makes a good job. It’s the people and the pride you take from what you do.”
Boldyrev’s experience with her son has given her a unique perspective for the patients and families she serves in the PICU.

“You don’t know anything about what it’s like if you’ve never had an unhealthy child. When my son was born, it opened a new world. I didn’t even know what congenital heart disease was, but now it’s unfathomable that I didn’t know,” she said. She recognizes that working in health care can be challenging, but it’s also the most rewarding thing she’s ever done. “If you’re passionate about medicine and helping people, but you’re hesitant to start the journey into health care, I say put your fears aside and take that first step.” Being able to provide compassion and support to children and families is something she’s very proud of, and she’s glad she took that first step. “I can be there for families going through the same type of situation I experienced,” Boldyrev said. “I feel like I’m able to make a difference in their lives. I believe there are reasons why we’re set on a path, and I take a lot of pride in saying that I’m a nurse.”
Read more
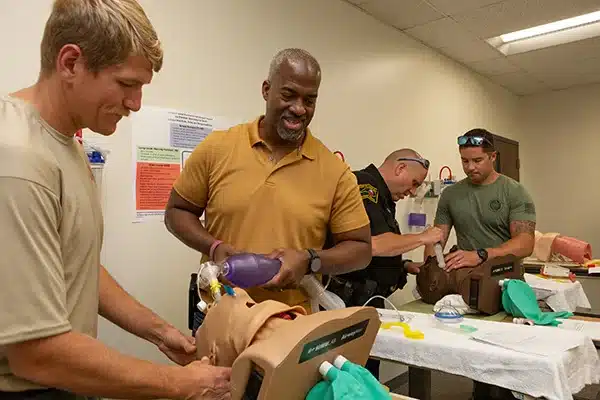
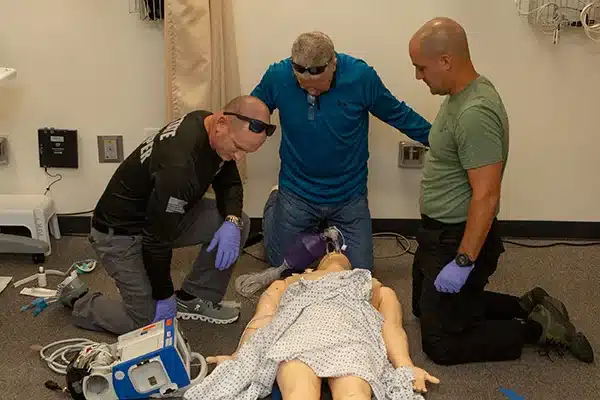
The clinical simulation center at East Carolina University’s Brody School of Medicine is usually peopled with fresh-faced students in scrubs and running shoes with tousled college-kid hair.
During the first week of the fall 2023 semester, however, the trainees in the school’s simulation center wore T-shirts with state trooper logos and utility belts on their hips.
On Aug. 23, the Brody simulation center welcomed more than 40 members of North Carolina’s law enforcement and first responder community to refresh their medical skills ranging from how to treat burns and heart attacks to the basics of assisting in an unplanned birth on the side of the highway.
Sean Johnson is North Carolina’s State Highway Patrol (SHP) director of training and manages more than 1,700 state troopers who need medical refresher training annually to stay qualified for their positions. Johnson, who worked the road for years before assuming his new role, knows from first-hand experience that being proficient in basic emergency medical response as a law enforcement officer is crucial because a car accident or other catastrophe could literally be just around the corner.
The highway patrol’s medical director — a doctor who oversees nine state government agencies including the Office of the State Fire Marshal, State Bureau of Investigation and Wildlife Resources Commission — has statewide jurisdiction to render medical care, making the SHP unique among first responders in North Carolina.
Johnson said that one of his urgent concerns is making sure that troopers are able to provide medical care before EMS workers arrive because of the uptick in the number of assaults on law enforcement officers in recent years, which might result in troopers rendering aid to those who tried to assault them. About a month ago, Johnson said, a law enforcement officer stopped to help a motorist change a tire and was shot by a career criminal.
“His vest saved him; He shot him with a .44 Magnum. But as soon as the trooper shot the suspect, he transitioned into patient care and tried to treat the guy. That’s the way we train them,” Johnson said.
The more common occurrences of vehicle accidents can be no less stressful and could require a Swiss army knife of medical response skills on a daily basis.
“You could go around a curve and there is a car wrapped around a tree and 911 has not even been activated so you’re talking about 10 to 15 minutes of waiting or treating somebody by yourself until higher level care gets there,” Johnson said. “Keeping these folks trained with the ability to deliver patient care is very important and we’re trying to grow our system.”
Johnson said one of the skills that annual training, like his troopers received at Brody, has improved upon is helping law enforcement to distinguish between a person who is experiencing a medical emergency, like a stroke or medicine imbalance, rather than being impaired behind the wheel.
“Troopers may stop somebody they think is drunk when they’re having a diabetic emergency or won’t respond, they may be having a complex partial seizure,” Johnson said. “Training in a controlled environment, where feedback can be given, is a game changer for public safety.
“The community is very appreciative when they get to see a side of a trooper that they’re not expecting. This is definitely beneficial to everybody.”
Value of training
Joe Bright Jr. spent most of his career with the State Highway Patrol protecting the N.C. State football team and its coach, but he bleeds purple and gold. He was an outside linebacker for the ECU football team in the run up to the Peach Bowl win in 1992 and after graduation was hired to provide security at the Brody School of Medicine while he completed law enforcement training. After a year with the ECU Police Department he moved to Raleigh and started working as a state trooper.
Bright said the training he received prepared him for the few instances where he was called upon to provide medical aid in uniform, but as a public servant his responsibility to the public didn’t end when he took his uniform off.
“Ask my wife. When I’m at Walmart or on the side of the road, just knowing what to do when someone has a medical emergency is important,” Bright said. “I use these skills for my safety team at church. Anytime we learn as officers and first responders the best thing for us to do is share that knowledge.”
Rebecca Gilbird, administrative director of Brody’s clinical simulation program, said the school has been working for several years to partner with the highway patrol to get troopers into the school for refresher medical training. The training is a public service that meet’s Brody’s mission of caring for the people of eastern North Carolina.
Brody’s simulation program is usually booked a year in advance because it primarily exists to train ECU medical and allied health students, medical residents and hospital staff, so getting a free day to accommodate law enforcement and first responder training is a rare luxury, Gilbird said.
“We started working with the state highway patrol last November; that’s how long we’ve had this on our calendar. We reserved the date and they’re coming back in November to do another round,” Gilbird said.
Benefit for the state
Lee Kennedy works for the Office of the State Fire Marshal. For his day job he assesses response capabilities of fire departments across a broad swath of southeastern North Carolina. He is often deployed to support state agencies during hurricanes and other natural disasters. In his spare time, Kennedy volunteers as a fire chief in Faison.
“In my six years working for the state I’ve had it a couple of times where we’ve ended up having somebody get too hot or somebody having chest pains,” Kennedy said.
Kennedy said the dynamic mannequins used in medical training scenarios at Brody — the ones that respond to questions and present trainees with true vital signs — makes training more realistic and valuable to law enforcement and other state workers.
“Normally it’s just talking through situations or treating a mannequin that doesn’t respond so that was actually pretty cool,” Kennedy said.
Bright, the state trooper who finished his career as the first sergeant of the SHP Training Academy, said that while it’s not the primary responsibility of law enforcement to provide first aid in the field, the confidence that comes from keeping basic skills refreshed is invaluable, particularly in rural areas of the state.
“Some officers may be the first one on the scene and knowing what to do for someone who needs medical attention makes us feel that much more confident in our work,” Bright said.
Kimberly Farmer is relatively new to the highway patrol, having worked more than three years in Harnett County where she grew up, but has been an EMT for more than seven years. While the county is fairly rural, Farmer said, first responders usually make it to incidents that require medical intervention before she does. However, being trained and having periodic refresher training like the kind she received in Brody’s simulation center, gives her confidence to know how to care for those in dire medical circumstances.
“We’ve gone through a ton of scenarios in the short time that we’ve been here this morning. We really hadn’t been able to do this in the past couple of years which COVID played a large part in,” Farmer said.
Gilbird, the simulation center director, takes pride in helping members of another state agency be ready to care for those in need.
“It makes me feel good that we have trained personnel out there. If I get in a wreck or my parents get in a wreck — we’ve trained them,” Gilbird said.
On the afternoon of Monday, April 8, the skies over eastern North Carolina will offer a spectacular sight: a solar eclipse. However, ECU Health ophthalmologist Dr. Ann Ostrovsky emphasizes a crucial caution: never gaze directly at the eclipse without proper eye protection. Doing so risks severe and potentially irreversible damage to your vision and eyesight, even leading to blindness.
A solar eclipse happens when the moon blocks the sun from view over a period of a couple of hours.
According to Dr. Ostrovsky, looking directly at the sun during the eclipse can cause a burn to the retina, even after a few seconds. This damage can cause a range of vision impairments including color distortion and reduced clarity. This risk extends to viewing the sun through any optical aid such as camera lenses, telescopes or binoculars.

“The consequences of retina damage from direct eclipse viewing are often permanent, with symptoms appearing within a 24 hours,” said Dr. Ostrovsky.
However, there are safe methods to watch the eclipse. Specialized eclipse glasses or pinhole cameras provide effective protection. It’s important to note that eclipse glasses differ significantly from standard sunglasses.
Dr. Ostrovsky stresses the importance of using proper eclipse viewing equipment.
“Ensure you have certified solar eclipse glasses with the appropriate grading, and always inspect them for any signs of damage or wear before use,” said Dr. Ostrovsky.
Should you suspect any optical damage following the eclipse, immediately contact your eye care provider.
While the solar eclipse promises a memorable sight, remember to protect your eyesight should remain the foremost priority during this awe-inspiring event.
Pediatric patients at the Maynard Children’s Hospital at ECU Health Medical Center had an opportunity to get outside in beautiful spring weather and have a little fun with their care teams during a Jell-O toss event on Tuesday, April 2.
With doctors, nurses, therapists and more Maynard team members lined up in chairs, patients dipped their hands into bowls of Jell-O and tossed the snack onto their care teams.
For patients, it was an opportunity to get out of their rooms, see their providers in a new way and relieve some stress.
One parent, Jillian Berntsen, said the opportunity was invaluable for her daughter Ella. While she was hesitant about participating at first, her care team encouraged her to join the event. Jillian said her daughter was glad she attended – even if she was covered in Jell-O by the end.

“This is incredibly important. For children like Ella who have long stays here in the hospital, it’s really important to get the outside and thinking about something other than their diagnosis so that they can have those moments being a child again,” Jillian said. “She’s just 13 years old so being stuck in a hospital room for most of her day can be tough. Things like this that get her smiling, laughing and around others are really important.”
For Abby Coderre, a pediatric nurse at the Children’s Hospital, the event meant more to her than a few laughs with patients and fellow members of her care team as she was splattered with the green Jell-O.
In 2019, Coderre was a patient herself at ECU Health Medical Center with lymphoma and shared a special relationship with her care team. She said passing on her experience as a patient to those she cares for now is crucial and these events give her a chance to connect with her patients in a different way.
“It’s great to give them an outlet and something fun to do while they’re at the hospital,” Coderre said. “Anything to make them smile, I would do it. It’s just a great opportunity to get to know these kids and continue to build that relationship.”
Ella Berntsen was diagnosed with leukemia in November and recently had an infection which led to eight surgeries. Her mother, Jillian, said the care teams at Maynard Children’s Hospital have been a difference-maker for her daughter and the connection she has to the care team is special.
“We feel so supported by all of the staff here, I can’t compare them with anything,” Jillian said. “The relationships and bonds we have formed with these people throughout this short period of time have been unbelievable – they’re like family to us. Ella has been through an incredible struggle, for me there has been a lot of doubt. To have these moments of happiness, it’s just really important.”
Further reading
Watch: Doctor and nurse share unique bond, respect after life-saving encounter


