Ahoskie, N.C. – ECU Health Roanoke-Chowan Hospital has earned recertification as a primary stroke center by The Joint Commission and the American Heart Association/American Stroke Association, recognizing the hospital’s preparedness and expertise to care for stroke patients.
“I am proud of ECU Health Roanoke-Chowan’s team members and their commitment to provide high-quality stroke care to our patients and community,” said Brian Harvill, interim president of ECU Health Roanoke-Chowan, president of ECU Health Chowan Hospital and ECU Health Bertie Hospital. “Our hospital’s stroke recertification as a primary stroke center from The Joint Commission – and stroke readiness at each ECU Health hospital – represents ECU Health’s dedication to bringing a comprehensive stroke network to care for all patients across eastern North Carolina.”

Stroke is a leading cause of death in North Carolina and the leading cause of long-term disabilities. As a primary stroke center, ECU Health Roanoke-Chowan can treat and stabilize patients experiencing an acute stroke and care for more complex cases. Located in Ahoskie, North Carolina, ECU Health Roanoke-Chowan serves a rural community and is the closest emergency department for surrounding communities. As a resource for emergency care, ECU Health Roanoke-Chowan’s recertification ensures local community members have access to timely stroke care and extends the comprehensive stroke network capable of meeting the needs of all patients across eastern North Carolina.
The likelihood of having a stroke in North Carolina is significantly higher than the rest of the country as a whole. North Carolina is about 8 percent worse for stroke mortality than the national average, and in eastern North Carolina, that risk is even greater.
“Time is the most important factor when treating a stroke, so it is critical to provide stroke care close to home,” said Dr. Barry Bunn, regional emergency department medical director, ECU Health. “With eastern North Carolina’s high rates of stroke, ECU Health Roanoke-Chowan’s stroke recertification, combined with a network of stroke readiness at all ECU Health hospitals, reduces the time of treatment, the risk of mortality, permanent brain damage and other side effects including memory loss, difficulty speaking and potential paralysis.”
During the certification process, ECU Health Roanoke-Chowan was evaluated on performance measures in stroke care, including education for patients and families on stroke risk factors and recognizing symptoms of stroke. Other performance measures included staff education on stroke protocols and the appropriate prescription of medications to address stroke risk factors such as elevated cholesterol and blood pressure.
Roanoke Rapids, N.C. – The Joint Commission and the American Heart Association/American Stroke Association has recertified ECU Health North Hospital as a primary stroke center by recognizing the hospital’s preparedness and expertise to provide timely and high-quality care for stroke patients.
“I am grateful to our team members across all levels and services for their commitment and diligent work that allows ECU Health North to continue to be designated a primary stroke center,” said Jason Harrell, president of ECU Health North Hospital. “Providing high-quality stroke care close to home is central to our mission of improving the health and well-being of eastern North Carolina. We are proud to be part of the top-notch neurological services provided at ECU Health across the region, which includes a strong network of expert stroke care.”

Stroke is a leading cause of death in North Carolina and the leading cause of long-term disabilities. According to the North Carolina Department of Health and Human Services, both Halifax and Northampton counties have higher incidences of strokes compared to the North Carolina average. As a primary stroke center, ECU Health North can treat and stabilize patients experiencing an acute stroke and care for more complex cases. As part of stroke readiness by all hospitals in the ECU Health system, this certification is symbolic of a comprehensive stroke network capable of meeting the needs of all patients across eastern North Carolina.
The severity and likelihood of having a stroke in North Carolina is significantly higher than the rest of the country as a whole. North Carolina is about 8 percent worse for stroke mortality than the national average, and in eastern North Carolina, that risk is even greater.
“Immediate treatment of strokes can minimize the long-term effects of a stroke and even prevent death,” said Dr. Barry Bunn, regional emergency department medical director, ECU Health. “With our region’s high rates of stroke and mortality from stroke, ECU Health North’s stroke recertification demonstrates our proven results of reducing the time of treatment, risk of mortality, permanent brain damage and other disabilities.”
During the certification process, ECU Health North was evaluated on performance measures in stroke care, including education for patients and families on stroke risk factors and recognizing symptoms of stroke. Other performance measures included staff education on stroke protocols and the appropriate prescription of medications to address stroke risk factors such as elevated cholesterol and blood pressure.
Survivors of stroke and brain injury had an opportunity to artistically express their journey during a recent Unmasking Brain Injury event at ECU Health Medical Center.
The Brain Injury Association of North Carolina sponsored the Unmasking Brain Injury workshop. This event provides blank face masks and supplies to decorate the masks. Unmasking Brain Injury is an organization that aims to bring awareness to the prevalence of brain injuries and give survivors a voice and the means to educate others of what it’s like to live and recover with a brain injury. The event was the first of its kind in the ECU Health system.
Michele Horvath, stroke navigator at ECU Health Medical Center, helped run the event and said it was a wonderful moment to share with survivors.
“Everybody was really engaged and it was an emotional time for survivors because it made them artistically express their stroke or their traumatic brain injury and some of them are still in recovery,” Horvath said. “They’re really excited to share their story and it was really heartfelt. We’re hoping to bring community awareness to some of these brain injuries.”

Along with a support person, each attendee, many of them members of ECU Health’s Stroke Support Network, decorated a mask to represent their journey and recovery process from their stroke or brain injury.
Molly Twiss, marketing coordinator at the Brain Injury Association of North Carolina, said it was the first Unmasking Brain Injury event she’d helped coordinate and she felt inspired after the event. She explained that the masks could be anything attendees wanted, not just their brain injury or stroke, but about themselves as a whole.
“The masks are a look inside of them, what they’re feeling, what they’ve gone through, what they hope for the future,” Twiss said. “Some can be as small as their favorite TV show, their favorite color or something about what their life was like before their injury. So if they were a skier beforehand and their accident was a ski accident, they can have it ski related. The mask could represent just something to get their mind off of having this invisible injury.”
Discovering New Passions
Wendy Gardner had her first child in 2000. Ten days after her son was born in Wilson, she suffered a hemorrhagic stroke, which has affected the left side of her body.
About a year ago, Gardner joined the Stroke Support Network at ECU Health and she said she’s enjoyed connecting with people in eastern North Carolina who have had similar experiences. She said the Unmasking Brain Injury event was a positive experience for everyone and she hopes for similar events through the support group in the future.
Gardner’s mask was painted red white and blue and adorned with a gold medal, representative of her new found passion — and talent — for archery.
About three years ago, Gardner stumbled upon archery as a sport she could participate in. Today, Gardner is a member of the USA Para Archery World team.

“I hadn’t been able to find a sport that I can do because my whole left side of my body is affected,” Gardner said. “So I can’t run and I really can’t swim and do the usual activities. So I’d kind of given up actually finding something that I could do. We happened to go to a big archery competition because our daughter was interested in it. I saw a guy who has no arms and shoots with his feet and his name is Matt Stutzman. He’s on our team. That is what got me inspired. I thought, if he can do it with no arms and I have one arm I could use, we could find some way for me to do this.”
Wendy and her husband went to work on figuring out some adaptive equipment to help her hone her new craft. She said there are not many resources available to help people with making adaptive archery equipment so they went through a “trial and error” process.
Once the Gardner family got a handle on making adaptive equipment and realized how expensive it could be for others to create their own equipment, they started a nonprofit called GX4 Adaptive Archery.
Her attitude since first suffering her stroke has made all the difference. She said she never expected to be involved in something like the USA Archery Team, and through her determination to try new things—coupled with her relentless effort—Gardner now travels the world doing something she loves.
This includes trips to the United Arab Emirates, Chile and Czech Republic with the team, and she hopes to be in France next summer for the 2024 Paralympic Games.
“I’m always like, ‘Why not me?’ And I would never have done anything like this if this had not happened to me,” Gardner said. “So I always tell people, go try something new. The main thing is show up, you’ve got to show up and don’t be afraid to look foolish doing it. Because sometimes, as someone with a physical disability, you will. But just show up and try and do your best.”
Resources
Stroke Support Network – Upcoming Events
Greenville, N.C. – ECU Health hospitals have received several American Heart Association/American Stroke Association Get With The Guidelines® achievement awards for their work in treating stroke, diabetes, cardiac arrest, heart attack, and heart failure.
These awards recognize the hospital’s commitment to ensuring patients receive the most appropriate treatment according to nationally recognized, research-based guidelines based on the latest scientific evidence.

“ECU Health’s recognition by the American Heart Association/American Stroke Association through the Get With The Guidelines® awards further demonstrates our commitment to providing high quality care across the region,” said Teresa Anderson, PhD, RN, NE-BC, senior vice president of quality at ECU Health. “Meeting our mission to improve the health and well-being of eastern North Carolina is about creating solutions for chronic conditions that affect so many in our communities, from children, to adults, to the elderly. I am proud of the care teams recognized for their work in delivering excellent care.”
ECU Health hospitals receiving recognition include:
Hospital
Program
Awards
Stroke
Gold Plus
Target Type 2 Diabetes Honor Roll
Stroke
Gold Plus
Target Stroke Elite Plus Honor Roll
Target Stroke Advanced Therapy Honor Roll
Target Type 2 Diabetes Honor Roll
Stroke
Gold Plus
Target Stroke Elite Honor Roll
Target Type 2 Diabetes Honor Roll
“We are incredibly pleased to recognize ECU Health for its commitment to caring for patients with stroke,” said Steven Messe, M.D., chairperson of the Stroke System of Care Advisory Group. “Participation in Get With The Guidelines® is associated with improved patient outcomes, fewer readmissions and lower mortality rates- a win for health care systems, families and communities.”
Stroke, diabetes and cardiovascular disease, which includes heart failure, heart attack and cardiac arrest, are among the leading causes of death in the nation. Cardiovascular disease claims more lives each year than all forms of cancer combined and is a major cause of disability.
The American Heart Association considers diabetes one of the eight major controllable risk factors for cardiovascular disease (CVD). In fact, people living with Type 2 diabetes are two times more likely to develop and die from cardiovascular disease, such as heart attacks, strokes and heart failure than people who don’t have diabetes.
According to the American Heart Association/American Stroke Association, stroke is the No. 5 cause of death and a leading cause of adult disability in the United States. The severity and likelihood of having a stroke in North Carolina is significantly higher than the rest of the country as a whole.
“These awards are another proud moment for the ECU Health system as it earns the recognition from American Heart Association/American Stroke Association for providing a high level of stroke, diabetes and cardiac care,” said Dr. Niti Armistead, chief medical officer, ECU Health. “We are proud of our care teams for demonstrating best practices and delivering life-saving care for the patients we serve. These awards are a testament to team members across the region who embody ECU Health’s commitment to improve the health and well-being of eastern North Carolina.”
Washington, N.C. – ECU Health Beaufort Hospital – a campus of ECU Health Medical Center has been designated as a primary stroke center by The Joint Commission and the American Heart/Stroke Association, recognizing the hospital’s preparedness and expertise to care for stroke patients. Stroke is one of the leading causes of death in the state, resulting in more serious long-term disabilities than any other disease. With this designation, all ECU Health hospitals are equipped to provide advanced stroke care in communities across eastern North Carolina.
“Stroke certification from The Joint Commission represents ECU Health Beaufort’s commitment to provide high-quality stroke care to not only patients experiencing stroke symptoms, but to all of our patients,” said Debra Hernandez, president of ECU Health Beaufort. “We are proud of being designated a primary stroke center. The commitment and diligent work of team members across all levels and services made this a reality.”

As a primary stroke center, ECU Health Beaufort can treat and stabilize patients experiencing an acute stroke and care for more complex patients. As part of stroke readiness by all hospitals in the ECU health system, this certification is symbolic of a comprehensive stroke network capable of meeting the needs of all patients across eastern North Carolina.
“Achieving stroke certification for all nine hospitals has been our goal since launching an intentional focus on improving stroke care in eastern North Carolina seven years ago,” said Barry Bunn, chief of medical staff and regional medical director of emergency services, ECU Health. “At the start of this process, ECU Health began a pathway of certifying all of the ECU Health hospitals with some level of stroke certification by the Joint Commission. Stroke certified hospitals were prevalent west of I-95, but there were few certified hospitals in the eastern part of the state. Now, we can proudly say that patients across the region will have access to high-quality stroke care, regardless of where they live.”
Because time is one of the most important factors in treating stroke, it is vitally important to provide stroke care close to home. ECU Health Beaufort’s stroke certification increases proximity to quality care in the Washington area, which reduces the risk of mortality, permanent brain damage and other side effects including memory loss, difficulty speaking and potential paralysis.
During the certification process, ECU Health Beaufort was evaluated on performance measures in stroke care, including education for patients and families on stroke risk factors and recognizing symptoms of stroke. Other performance measures included staff education on stroke protocols and the appropriate prescription of medications to address stroke risk factors such as elevated cholesterol and blood pressure.
The severity and likelihood of having a stroke in North Carolina is significantly higher than the rest of the country as a whole. Eastern North Carolina is at the center of many strokes, often called the buckle of the stroke belt. North Carolina is about 8 percent worse for stroke mortality than the national average, and in eastern North Carolina, that risk is even greater.
“With all hospitals in the ECU Health system now stroke certified, a patient will be offered life-saving care regardless of the patient’s proximity to any of ECU Health’s hospitals and depending upon what additional treatments are needed, can be transported to a location with more extensive services when the patient is stabilized,” said Jay Briley, president of ECU Health Community Hospitals. “This system-wide stroke certification helps fulfill ECU Health’s mission of improving the health and well-being of eastern North Carolina.”
Younger people are increasingly suffering from strokes according to medical experts at ECU Heath. While risk of stroke increases with age, health care teams have seen an increase in strokes in young people, partly due to a combination of COVID-19, an increase in consuming processed, sugary and fatty foods as well as smoking and vaping.
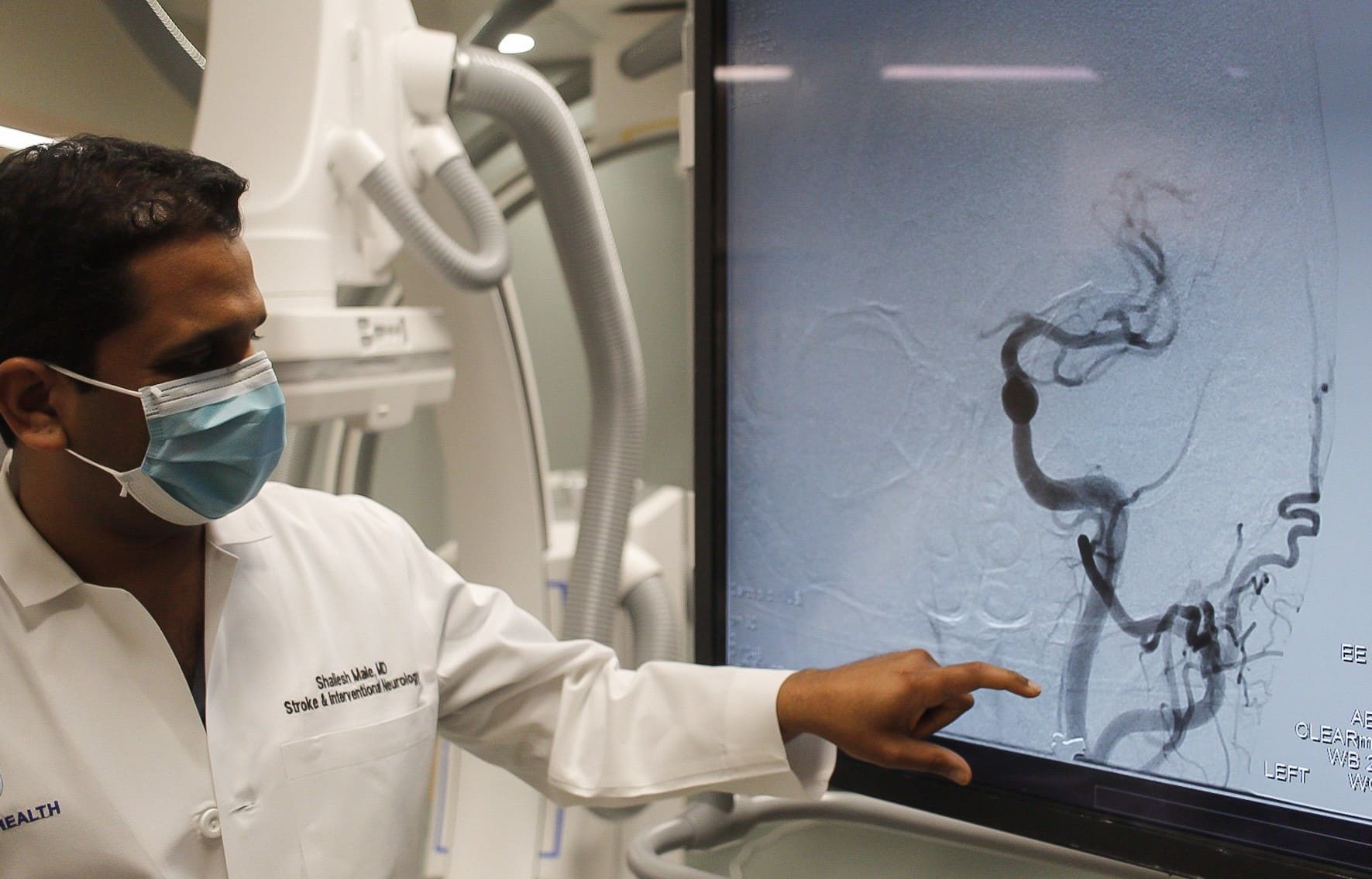
“With COVID-19, we have noticed an increase in strokes, especially in younger populations,” said Dr. Shailesh Male, stroke medical director, ECU Health Medical Center. “During the peak of the pandemic, my colleagues and I noticed that young patients who do not have vascular risk factors were having strokes. COVID-19, like other infections, increases the risk of forming blood clots and, in turn, can lead to higher risk of strokes.”
Strokes are considered the heart attack of the brain. A stroke occurs when a blood clot compromises blood flow to the brain. This leads to loss of brain function, manifesting in symptoms including: weakness or numbness on one side of your body, slurred speech or difficulty understanding others, blindness in one or both eyes, dizziness and/or a severe headache.
Risk factors for stroke can be broken down into two categories: modifiable and non-modifiable.
“We like to focus on the modifiable risk factors, the ones that you can change,” said Dr. Male. “These include hypertension, cholesterol, diabetes, smoking, physical inactivity and obesity.”
The increase in younger people having strokes are mostly attributed to modifiable risk factors. The rise in popularity of e-cigarettes and vaping has largely been in younger populations. Smoking reduces the amount of oxygen in the blood, makes the heart beat faster and raises blood pressure. Additionally, younger people are generally less healthy than previous generations in terms of diet and exercise.
“Processed, fatty and sugary foods are increasingly becoming a regular part of our diets at a younger age,” said Dr. Male. “This combined with an inactive lifestyle increases almost all risk factors including obesity, diabetes, high blood sugar, hypertension and high cholesterol.”
Non-modifiable risk factors include older age, gender (men face higher risk of stroke), family history, genetics and even race. According to The Office of Minority Health, African Americans are 50 percent more likely to have a stroke than non-Hispanic whites adult counterparts and 70 percent more likely to die from a stroke.
“African Americans have higher incidences of hypertension, diabetes and high cholesterol, which in combination, increases the risk of strokes,” said Dr. Male.
It is important to discuss risk factors with your primary care provider. If you have had a stroke, your doctor may prescribe preventative medications to address risk factors like blood thinners, cholesterol medication or blood pressure medication. Additionally, lifestyle changes such as exercising more and eating healthier foods are proven to lower your risk of stroke.
“With great treatment options now widely available, it is important to remember, time is of the essence,” said Dr. Male. “The sooner we implement treatment, the better the odds that the patient will recover to their baseline. The benefit of early treatment is preventing long-term disability.”
If a stroke is not caught quick enough, long-term disability and health issues are possible. Most commonly, patients may lose strength on one side of their body or have problems speaking.
The acronym B.E. F.A.S.T. can help quickly identify the signs and symptoms that you or a loved one may be experiencing a stroke:
- B – Balance problems
- E – Eye issues like blindness or seeing doubles
- F – Face drooping
- A – Arm weakness
- S – Speech slurring
- T – Time to call 911
 Greenville, N.C. – October 11, 2021– Vidant Health hospitals have received several American Heart Association/American Stroke Association Get With The Guidelines® achievement awards for their work in treating stroke, diabetes, cardiac arrest, heart attack, and heart failure.
Greenville, N.C. – October 11, 2021– Vidant Health hospitals have received several American Heart Association/American Stroke Association Get With The Guidelines® achievement awards for their work in treating stroke, diabetes, cardiac arrest, heart attack, and heart failure.
These awards recognize the hospital’s commitment to ensuring patients receive the most appropriate treatment according to nationally recognized, research-based guidelines based on the latest scientific evidence.
“Vidant’s recognition by Get With The Guidelines® demonstrates our commitment to quality care. Meeting our mission to improve the health and well-being of eastern North Carolina means finding solutions for chronic conditions that affect so many in our region, “ said Teresa Anderson, PhD, RN, NE-BC, senior vice president of quality at Vidant. “The Vidant system is proud to be recognized by the American Heart Association for turning guidelines into lifelines.”
Vidant Health hospitals receiving recognition include:
Vidant Beaufort Hospital, a campus of ECU Health Medical Center — Stroke Gold Plus and Target Type 2 Diabetes Honor Roll
Vidant Chowan Hospital — Stroke Gold Plus and Target Type 2 Diabetes Honor Roll
Vidant Duplin Hospital — Stroke Silver Plus and Target Type 2 Diabetes Honor Roll
Vidant Edgecombe Hospital — Stroke Gold Plus and Target Type 2 Diabetes Honor Roll
ECU Health Medical Center — Stroke Gold Plus and Target Stroke Elite Plus Honor Roll, Target Type 2 Diabetes Honor Roll, Mission: Lifeline Award: Gold Receiving, and Mission: Lifeline NSTEMI: Gold
Vidant North Hospital — Stroke Silver Plus and Target Type 2 Diabetes Honor Roll
Vidant Roanoke-Chowan Hospital — Stroke Gold Plus, Target Stroke Honor Roll and Target Type 2, and Diabetes Honor Roll
The Outer Banks Hospital — Stroke Gold Plus and Target Stroke Honor Roll Elite
“We are pleased to recognize Vidant Health for their commitment to diabetes, stroke and heart care,” said Lee H. Schwamm, M.D., national chairperson of the American Heart Association’s Quality Oversight Committee and executive vice chair of neurology, director of Acute Stroke Services, Massachusetts General Hospital, Boston, Massachusetts. “Research has shown that hospitals adhering to clinical measures through the Get With The Guidelines® quality improvement initiative can often see fewer readmissions and lower mortality rates.”
Stroke, diabetes and cardiovascular disease, which includes heart failure, heart attack and cardiac arrest, are among the leading causes of death in the nation. Cardiovascular disease claims more lives each year than all forms of cancer and chronic lower respiratory disease combined.
According to the American Heart Association/American Stroke Association, stroke is the No. 5 cause of death and a leading cause of adult disability in the United States. On average, someone in the United States suffers a stroke every 40 seconds and there are nearly 795,000 new or recurrent strokes each year. Stroke kills about 140,000 Americans each year, accounting for one out of every twenty deaths. In eastern North Carolina, the stroke death rate is even higher, highlighting the need for preventative and rapid care.
“These awards are another proud moment for the Vidant Health system as it earns the recognition from AHA/ASA for providing the highest level of stroke care through its network of acute stroke ready hospitals, primary stroke centers and a comprehensive stroke center,” said Dr. Shailesh Male, stroke medical director at VMC. “This honor is a testament towards Vidant’s commitment to improve the health and well-being of eastern North Carolina.”
To speak with a Vidant neurologist for non-emergency care, please call 252-816-9700.
To find a heart and vascular provider, please visit Vidanthealth.com/Find-A-Doctor
Dr. Dalyai joined WITN during Stroke Awareness Month in May to discuss stroke issues in the area.
“People here in North Carolina are so much more likely to have a stroke and to die from a stroke than elsewhere in the country,” Dr. Dalyai said, “and even more so in eastern North Carolina than other parts of North Carolina.”
There are many different factors that can lead to stroke, including hypertension, or high blood pressure, smoking and diets that are high in fat. There is also a genetic component and there is a racial disparity in that strokes are more common in African Americans.
To spot the signs of a stroke, it is important to remember the acronym B-E F-A-S-T.
B – Balance, watch for a loss of balance
E – Eyes, vision changes
F – Face drooping
A – Arm weakness
S – Speech difficulty
T – Time to call 911
Dr. Dalyai said there are a number of ways to prevent stroke, depending on your risk factors. He said talk with your primary care provider to determine your risk and what you can do to stay healthy.
“The biggest thing that we tell patients is that they really should work with their primary care provider to focus on their specific needs,” Dr. Dalyai said. “Whether it’s medications or diet, physical activity, all these things that are specific to you that you can do to reduce your risk of having a stroke.”
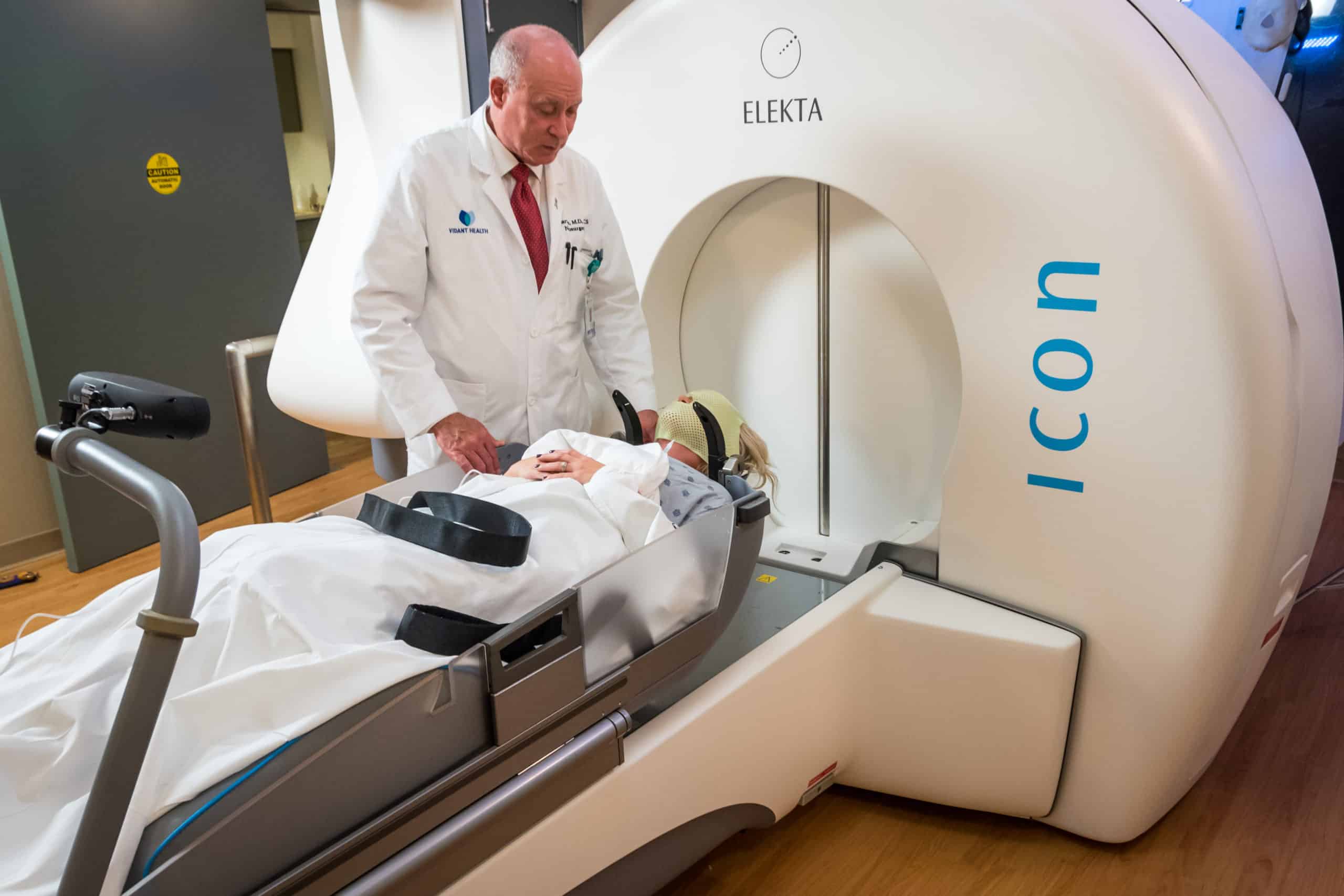
ECU Health Medical Center passes 2,000 Gamma Knife treatments

ECU Health Medical Center (VMC) was proud to recognize its 2,000th Gamma Knife treatment in April.
“I am incredibly proud of this important milestone in Vidant’s collective work to realize a life without cancer,” said Dr. Stuart Lee, chief, division of neurosurgery, Vidant Health and medical director of The Gamma Knife Center, VMC. “Our teams work passionately to support those battling cancer. Those across our region can access advanced technology close to home, which reduces the need to travel elsewhere to receive treatment. By performing 2,000 Gamma Knife® procedures, we are delivering on our mission to improve the health and well-being of eastern North Carolina.”
The Gamma Knife® at VMC is one of only two in North Carolina and the newest version, the Gamma Knife®ICON, was installed in 2018. The Gamma Knife® works by destroying cancer cells, which shrinks the size of brain tumors over time. This technology offers quick recovery time and can be done in an outpatient setting, preventing the need for hospitalization. Gamma Knife® also provides convenience by requiring minimal follow-up procedures, reducing barriers related to travel for the patient.
“On behalf of ECU Health Cancer Care, I want to express my sincere gratitude to Dr. Lee and his team,” said Chris Wood, senior administrator, ECU Health Cancer Care. “Nearly all of us are impacted in some way by cancer, whether it’s through our own personal experiences, or the experiences of a loved one. Dr. Lee and his team are an important part of how ECU Health Cancer Care provides for those we love and serve who are battling cancer.”
To learn more about the full spectrum of Neurological Care, including neurology and neurosurgery, visit VidantHealth.com.
 Roanoke Rapids, N.C. – July 15, 2021 – Vidant North Hospital is proud to announce it has been designated as a primary stroke center by The Joint Commission and the American Heart/Stroke Association, recognizing the hospital’s preparedness and expertise to care for stroke patients. Stroke is one of the leading causes of death in the state, resulting in more serious long-term disabilities than any other disease.
Roanoke Rapids, N.C. – July 15, 2021 – Vidant North Hospital is proud to announce it has been designated as a primary stroke center by The Joint Commission and the American Heart/Stroke Association, recognizing the hospital’s preparedness and expertise to care for stroke patients. Stroke is one of the leading causes of death in the state, resulting in more serious long-term disabilities than any other disease.
According to the North Carolina State Center for Health Statistics, both Halifax and Northampton counties show increase incidences of stroke disease and mortality compared to the North Carolina average. “Here in eastern North Carolina we are at the center of a lot of strokes. North Carolina is about 8 percent worse for stroke mortality than the rest of the nation and in eastern North Carolina it is even a bigger risk,” said Dr. Richard Dalyai, neurosurgeon and surgical director of stroke services at Vidant Health. “Providing high-quality stroke care close to home is central to our mission of improving the health and well-being of eastern North Carolina.”
As a primary stroke center, Vidant North can treat and stabilize patients experiencing an acute stroke and care for more complex patients. Because time is one of the most important factors in treating stroke, it is vitally important to provide stroke care close to home. Vidant North’s stroke certification increases proximity to quality care in the Roanoke Rapids area, which reduces the risk of mortality, permanent brain damage and other side effects including memory loss, difficulty speaking and potential paralysis.
During the certification process, Vidant North was evaluated on performance measures in stroke care, including education for patients and families on stroke risk factors and recognizing symptoms of stroke. Other performance measures included staff education on stroke protocols and the appropriate prescription of medications to address stroke risk factors such as elevated cholesterol.
“Stroke certification from The Joint Commission represents Vidant North Hospital’s commitment to provide high-quality stroke care to not only patients experiencing stroke symptoms, but to all of our patients,” said Jason Harrell, president of Vidant North. “We are proud of being designated a primary stroke center and the commitment and diligent work of our team members across all levels and services to make this a reality.”
“I am incredibly proud of this important milestone in Vidant’s collective work to realize a life without cancer,” said Dr. Stuart Lee, chief, division of neurosurgery, Vidant Health and medical director of The Gamma Knife Center, ECU Health Medical Center.
The Gamma Knife® works by targeting problematic cells, which shrinks the size of brain tumors over time. This technology shortens recovery time and is often performed in an outpatient setting. Before this technology, for certain kinds of brain tumors, the treatment was whole-brain radiation, which means even the healthy parts of the brain were radiated.
Dr. Lee spoke of a previous patient whose brain tumor shrunk significantly six weeks after treatment. “This was a lady in her late thirties who was still working, even with her cancer,” Lee said. “She actually went on a cruise after her second Gamma Knife®.”
“Our teams work passionately to support those battling cancer. Those across our region can access advanced technology close to home, which reduces the need to travel elsewhere to receive treatment,” said Dr. Lee. “By performing 2,000 Gamma Knife® procedures, we are delivering on our mission to improve the health and well-being of eastern North Carolina.”