The American Association of Cardiovascular and Pulmonary Rehabilitation’s (AACVPR) Day on the Hill, which was March 4-5 this year, is an opportunity for cardiac and pulmonary rehabilitation professionals to visit Washington, D.C. to advocate for their profession and ask legislators for support for beneficial legislation on Medicare decisions. It was Stacey Greenway’s 10th year participating in this event, a milestone made all the more significant by her recent election as treasurer to the AACVPR board.
Stacey, the director of cardiovascular disease management services at ECU Health Medical Center, wasn’t initially interested in health care policy, but her zeal for her work inspired her to get involved.
“I’m passionate about what I do, and when I realized the impact these legislative decisions make on our patients, I wanted to get involved,” she said. “When the North Carolina Cardiopulmonary Rehabilitation Association (NCCRA), which works on the state level, asked if anyone was interested in participating in Day on the Hill, I thought how cool it would be to help our patients and our programs. After the first time, I was hooked.”

Each year, the AACVPR’s legislative priorities are different, but the goal is the same. “We want to help the legislators see things from the patient perspective and put a face to the people these bills are affecting,” Stacey said. “From that angle, you see the increase in a patient’s quality of life. From a health system perspective, it decreases the rates of hospital readmission. It’s a win-win.”
This year’s priorities centered on two bills: HR-955/S.1849, the Sustaining Outpatient Services Act, and HR-1406/S.3021, the Sustainable Cardiopulmonary Rehabilitation Services in the Home Act. The Sustaining Outpatient Services Act seeks to correct a legislative error from a previous bill that reduces reimbursement for cardiac and pulmonary rehabilitation services when they are provided in off-hospital campus clinics. The reduced reimbursement rate makes cardiac and pulmonary rehabilitation services financially unsustainable and thus eliminates patient access to these resources, especially in rural communities. “Some rural hospitals, which don’t have a lot of real estate on campus, haven’t even tried to open a rehab clinic because of this issue,” Stacey said. This bill would establish an exemption status to certain hospital outpatient services, including cardiac and pulmonary rehabilitation, from that fee reduction.
The Sustainable Cardiopulmonary Rehabilitation Services in the Home Act would allow Medicare beneficiaries to receive cardiac or pulmonary rehabilitation services through real-time telehealth in their homes. This hybrid type of service was very successful during the pandemic, and it allowed more patients to be treated from across eastern North Carolina.
“Think of that 45-year-old patient who had a heart attack and would benefit from rehab services but has also been cleared to work and needs to make an income,” Stacey explained. “This bill would allow that patient to not have to make a choice between income and health; they could do both.”
During her time in Washington, D.C., Stacey and 74 other AACVPR members spoke with their respective House Representatives and Senators to advocate for these bills. Stacey said overall, the discussions were productive.
“I had some good conversations about both bills,” she said. “The telehealth bill was one the legislators could wrap their heads around easier; it was something they were familiar with. That was encouraging.” While more work needs to be done to increase support for the outpatient services bill, Stacey said she felt the needle moved a bit. “This is partly because the government seems to be changing their focus from thinking about the up-front costs of health care to the savings incurred on the back end,” Stacey said. “That means things are changing, and I’m hoping we’ll get a few more co-signatures on that bill.”
As a board member, Stacey said she now has other opportunities to support her profession.
“To represent eastern North Carolina and discuss at the national level some of the things that impact those who practice locally is really important,” she said. Because she was on the board this year, Stacey was also able join the board meeting the day before Day on the Hill and participate in the selection of a new legislative firm. “We met with the firm and prepped for Day on the Hill, but we also strategically planned for the future,” Stacey said. “It was exciting to be involved in that process.”
Stacey’s interest in running for the AACVPR’s treasurer position stemmed from her desire to stay involved in the national organization and escalating care for patients.
“The board is involved in regulatory and government relations, and that’s one of my big interests. Day on the Hill is just one way we stay involved. It’s a way of understanding and supporting initiatives and bringing that back to ECU Health,” she said. “We have six cardiac and pulmonary rehab programs within ECU Health, and I want to make sure those programs are aware of the initiatives the AACVPR promotes to escalate their practice and ensure we’re doing the best we can for our patients.”
Now that the initial conversations with Congress members are over, the next step is to follow up in a few weeks with those representatives still on the fence. “We’ll also bring in a constituent from that person’s district to speak to the impact of these bills,” Stacey said. Some representatives have already signed on to at least one of the bills, including Rep. Don Davis, Rep. Deborah Ross, Rep. Greg Murphy, Rep. Wiley Nickel and Rep. Jeff Jackson.

It’s important to be involved in the policy issues surrounding health care, Stacey said. “You don’t go into health care thinking about these operational or political issues, but when you’re faced with the repercussions in the clinic, you see the impact it has.”
She encouraged all health care professionals to get involved: “Let’s do this for the betterment of the patient experience,” she said. “For me, this has been one of the highlights of my professional life.”
Tanya Graham, a North Carolina native and Greenville resident, was outside cutting her grass when she started to feel very tired. That night, she experienced what felt like an asthma attack, so the next day she visited an urgent care clinic. “I do have asthma,” Graham shared, “but I’ve never had an attack.” The doctor ran a few more tests, and after an EKG, he decided to send Graham to the hospital.
“The cardiologist at [ECU Health] Medical Center said, ‘You are in heart failure,'” Graham said. “I didn’t know what he was saying, I was so shocked.”
Dr. W. Douglas Boyd, a cardiothoracic surgeon, told Graham she needed surgery, and two weeks later, Graham found herself back in the hospital recovering from a double coronary bypass. She was told later that her initial ejection fraction, which is the amount of blood your heart pumps each time it beats, had been 10 percent. A normal ejection fraction is 50 percent or higher. “After the surgery, they did another echocardiogram, and now it’s up to 35 percent,” Graham said.

Graham knew that once she was strong enough after the surgery, she wanted to participate in cardiac rehabilitation. She had heard about the option from her neighbor, who also had recently suffered a heart attack. “I also have two sisters who are nurses,” Graham shared. “One of them works for a cardiologist, so I talked with her about cardiac rehab, and all of my siblings agreed it was a good idea.”
Cardiac rehabilitation focuses on the “what now” after a cardiac event. Stacey Greenway, the director for cardiovascular disease management services at the Medical Center, hopes that cardiac rehab will become the immediate program associated with cardiac recovery.
“A multidisciplinary team works with the patients to establish and achieve goals to improve their health, quality of life and functional ability,” Greenway said. “We develop individualized treatment plans for each patient that includes exercise, nutrition, medications, stress management and other components.”
For Graham, therapy started slow, but she said she immediately felt comfortable. “The team is so smart, and they are in tune with each individual person,” Graham said. “It made a huge difference because I learned right off that I could trust them. It made me want to go.”
It also helped to have others around her going through the same experience. “It didn’t matter if they were a man or woman or what race they were – we were all there for the same reason. Our bodies had broken in some way, and we were all there together for the same purpose of trying to survive and extend our lives,” Graham said. “I drew strength from them, because when I saw them working hard, it made me want to do the same.”
The experience didn’t just provide Graham with the chance to get stronger after a major surgery. “The one thing I came away with,” Graham said, “is hope. Hope that I’d live a longer life.” Graham said that it wasn’t just the exercise that encouraged her and helped her get better; it was also the classes they offered. “I learned quite a bit from the classes, which covered things like diet and coping with this diagnosis,” she said. Something Graham didn’t expect was having access to support from a therapist. “I’d had a hard experience with my surgery, so they put me in contact with Dr. Kari Kirian, and she worked wonders. I can’t say enough positive things about that experience.” Dr. Kirian is a cardiac psychologist embedded in the heart failure program – a critical member of the care team as it is not uncommon for patients to experience anxiety or depression after a cardiac event.
While she wished she could have participated for longer, Graham graduated from cardiac rehab with the ability to do the things she needs to do. “It allowed me to come home and do the things you take for granted, like clean the house or roll your hair,” Graham said. She also immediately joined a gym and signed up for personal training to continue her progress. “I left cardiac rehab on a Friday, and that following Monday I was at the gym,” Graham said. “It wasn’t mandated, but the cardiac rehab team provided me with information. My sister goes to a gym, so I decided to go there, and now I go every weekday. I will continue to exercise, think positive and eat right.”
Because she’s feeling so much better, Graham said she has plans for the future. “I’m going to work on making one of my bedrooms a storage space, and in the spring, I plan to paint a shed in the back yard,” Graham said. She also hopes to visit her daughter and grandchildren in Phoenix, Arizona next winter. In the meantime, Graham said she’s cleared it with her doctors to serve as a volunteer in the cardiac rehab unit. It’s one way she can share her experience and give back to the amazing Cardiac Rehab team for impacting her life in an incredible way.
“I don’t care what I do. I just didn’t want to leave there,” Graham said. “I love people, and I thought maybe if I was around people going through what I went through, I could tell them my story and help them.”
The VAD (Ventricular Assist Device) program at ECU Health Medical Center has recently undergone its fourth successful Joint Commission survey, receiving exceptional praise.
As the largest health care accrediting body in the nation, the Joint Commission emphasizes patient safety and quality of care. The Joint Commission surveys the program’s compliance every two years with more than 40 standards organized into six different chapters in the disease-specific care manual.
ECU Health Medical Center’s VAD program is led by a team committed to providing cutting-edge care for patients relying on ventricular assist devices. A ventricular assist device is a surgically implanted device that helps in the functioning of the heart‘s pumping mechanism. At the Medical Center, VAD patients are often cared for in the following specialized units: CVICU, CIU, CICU, ED and Medical Rehab.

The surveyors highlighted the VAD program’s holistic approach to patient care, acknowledging the dedication of the multidisciplinary team.
“The survey holds our VAD program accountable and ensures that we are providing the highest quality and safest care possible to our patients,” said VAD Coordinator Andrea Matthews. Reflecting on her own participation in the program, Matthews shared her appreciation. “Having the opportunity to be involved in this program and care for this specialized patient population is truly an honor.”
VAD Coordinator Emily Knight echoed this sentiment and emphasized that the resilience of patients and their families is what makes her job rewarding. Knight shared that she’s excited to see what the future holds for the program.
“I am thankful that ECU Health is able to provide this care and treatment close to home for the patients of eastern North Carolina,” Knight said. “I am excited to see the program grow and evolve to reach more patients in our community.”
Since its inception in 2017, ECU Health’s VAD program has grown significantly. The program has successfully implanted 71 left ventricular assist devices (LVAD) and currently cares for 43 patients. Courtney Saunders, advanced heart failure cardiologist, expressed her gratitude for the exceptional individuals within the VAD team who play a crucial role in the program’s success.
“It has evolved into the program it is through the individuals recognized by the surveyor developing a gold standard of LVAD care,” Saunders said. The surveyors specifically highlighted Dr. Tae Joon Lee, Dr. Kari Kirian and Terrani Moore.
Jay Briley, ECU Health Medical Center president, joined the surveyors in commending the team for their hard work in this achievement.
“The Joint Commission survey results demonstrate the program’s dedication to excellence, teamwork and patient-centered care,” Briley said. “Congratulations to all the teams involved in the successful survey.”

John Core had never heard of pulmonary rehabilitation until he needed it.
“I went to urgent care with what I thought was a bad cold,” Core said. “But my heart was racing so they sent me to the hospital.”
Once in the ECU Health Medical Center emergency department, Core said they were unable to get his 144 beat-per-minute heart rate down with medications; the next step was to perform an electrical cardioversion, which is where the heart is shocked to restore a normal rhythm.
“I wound up in the ICU and stayed in the hospital for two weeks,” Core said. “When I got out, I had trouble breathing and had to be on oxygen, which I hated.”
After a six-week recovery, during which time Core said he could barely walk, his doctor recommended he try pulmonary rehabilitation.
“I was encouraged that my doctor thought I was strong enough to go,” Core said. Upon arriving, Core immediately felt comfortable in the rehab setting. “They were supportive and guiding. They were wonderfully attentive, and their sense of humor and generosity with their time made it the best experience I’ve ever had in health care.”
Pulmonary Rehabilitation helps reduce and control breathing difficulties and other symptoms of lung disease, including asthma, chronic obstructive pulmonary disease or pulmonary hypertension. ECU Health’s Pulmonary Rehabilitation team strives to help patients achieve their highest level of independence and physical ability.
Initially, Core could only walk one lap around the therapy track with the assistance of oxygen before needing a rest; but week by week, he increased his distance. He was impressed by the rehab team’s consistent regimen and organization.
“You had a set routine every visit: sign a form, get weighed, take your blood pressure and then start your program.” The planning and tracked improvement helped drive him to want to go to therapy his prescribed three times every week. “They made me like exercise, when I hated exercise before. I used to think exercise was a waste of heartbeats.”
Core was also impressed by the pulmonary rehab team’s rigorous standards and attention to detail.
“At first, I couldn’t go to the grocery store because I couldn’t walk the aisles,” Core said. “Then I got the idea that I could lean on the cart and put my oxygen tank in the cart. I was so proud of myself.”
The next day, Core said he told his rehab therapist what he’d done.
“She said, ‘That’s not good enough.’ At first that hurt my feelings, but she was right. It pushed me to walk longer and harder.” Any time Core showed signs of fatigue, he was made to rest so they could monitor his oxygen saturation, which should be above 90%. “When they saw I was throwing PVCs [premature ventricular contractions] during my walk, they stopped therapy until I was cleared by my cardiologist,” Core said.
PVCs are extra, abnormal heartbeats that disrupt a normal heart rhythm.
One day, Core asked the rehab team if he could try walking two laps without oxygen.
“They agreed but monitored me very closely. After my first lap, I was at 90-91% oxygen, thank the Lord.”
From there, Core worked his way up to 11 laps just prior to graduation. Now, Core said he is feeling better than he did before his stay in the hospital.
“After graduating from pulmonary rehab, I joined the ECU Health Wellness Center, and I really enjoy swimming. I’ve lost over 30 pounds, I exercise regularly and I’m overall trying to improve how I live my life. I like where I’m at,” he said.
Core works at East Carolina University as a special assistant to the dean in the School of Dental Medicine, and he enjoys spending time with his wife of 32 years, his children and grandchildren. He’s also looking forward to a great grandchild on the way. This spring, he and his wife have plans to resume travel to visit his daughter and son-in-law in Charleston, South Carolina. Taking a trip like that wasn’t feasible prior to his experience with the amazing Pulmonary Rehab team.
“I had trouble walking; I couldn’t even walk a quarter of a mile,” Core said. “Pulmonary rehab helped me back. They know what they’re doing, and you can depend on them. To know that people care for you – it makes a difference. I can’t tell you how good they make you feel if you let them.”
Tony Parker has always been an active runner and has long supported the Greenville running and biking community. When he collapsed near the finish line of a 5K road race due to cardiac arrest, quick action saved his life.
Tony was scheduled to run the half marathon that morning back in March of 2021, but backed down to the 5K after his knee started bothering him. It also gave him the chance to run alongside his wife, Delia. It turned out to be a life-saving choice.
“If it weren’t for Delia and the fact that she knows CPR, I wouldn’t be here today,” Parker said. “And if it weren’t for the city of Greenville and the rescue paramedic squads with their AED (automated external defibrillator), I wouldn’t be here today.”
He said he remembers running ahead of his group, including his wife, in the last stretch of the run since his knee was feeling better than anticipated. He patted a young runner on the back to encourage them and then he collapsed.
Delia, a dental assistant with the Department of Veterans Affairs, was required to take CPR courses every three months as part of her job training. That morning, her training paid off in a way she never imagined.
“I got up to the corner and I heard somebody shouting, ‘Man down.’ And when I turned the corner, I was like, that’s Tony,” Delia said.
Delia yelled for someone to call 911 and checked her husband for a pulse, but found none. So she started CPR.
“No one tells you when you’re training on a mannequin that you’ll hear crunching. No one tells you on a mannequin that it’s a different feeling when you’re pushing on somebody’s chest. And it was a little freaky when I first did it, but I was able to stay where I was and to do the compressions,” Delia said. “Someone, ‘Angel,’ as he liked to call them, came up and said, ‘Can I help you?’ They took over and I did some breaths for him.”
Tony and Delia still have not been able to track down the mystery “Angel” from that morning who helped them with CPR.
Shortly after, paramedics arrived and took over. They told Delia that Tony had been revived and he was on his way to ECU Health Medical Center. Paramedics could quickly identify Tony and his wife because he was wearing a road ID, which gives paramedics information on a person, should an emergency event occur. Tony and Delia said they encourage people in their running and biking groups to wear a road ID for these situations.
Delia met Tony at the hospital and some tension was relieved when Tony greeted her with his nickname for her – “Hiya, toots.”
Tony spent about a week at the hospital while the care team ran tests and navigated next steps for the Parker family. They said their time at the hospital and in clinics since has been reassuring and helpful as Tony adjusted to his new normal.
“The care there was incredible. When I say care, I mean that as the word of choice. They really care about what they’re doing and they make sure that they take care of you,” Tony said. “For somebody with a personality like mine, they make sure I don’t try to overdo it right away. The follow up has been spectacular. They stay in contact with my primary care doctor so we’re all on the same page as to what’s going on. ECU Health has been incredible.”
Dr. Christopher Gregory, an interventional cardiologist with ECU Health, said cardiac arrest can come on with no symptoms in some patients and out-of-hospital cardiac arrests are very uncommon to survive due to how quickly care is needed in these cases. Though they may seem similar, Dr. Gregory said it’s important to know the difference between a heart attack and cardiac arrest.
“Heart attacks are when the blood flow to the heart, because of blockages in the arteries, generally speaking, that feed the heart, is impaired,” Dr. Gregory said. “That causes the heart muscle to be stressed, strain or even die – that’s a heart attack. Cardiac arrest is when the heart itself stops. Sometimes heart attacks cause cardiac arrest, but they are completely different.”
Today, Tony is back out walking, running and biking as often as possible. He’s involved in groups of athletes that have experienced heart attacks, cardiac arrest or other heart health challenges and he said this has given him a great perspective on his own journey. As an advocate, Tony meets with groups around the state to stress the importance of road IDs, greater access to AEDs and the need to stay active throughout your life.
“I would rather be an active participant in life than a passive participant and I’ve seen the difference it’s made in the lives of people around me,” Tony said. “My father was very active and his quality of life was excellent. He did have a stroke that impacted him, but he was still walking and getting out there. He played senior games basketball at 86 years old. So when you see the difference, you understand.”
Learn more about ECU Health Heart & Vascular Care.
Greenville, N.C. – Four ECU Health Physicians clinics have been recognized by the American Heart Association and American Medical Association for its commitment to improving blood pressure (BP) control rates, earning Gold-level recognition as part of Target: BP. The Gold award recognizes practices in which high blood pressure is controlled in 70% or more of the adult patients affected.
“Managing and controlling your blood pressure is essential for preventing the development of heart disease and stroke, which continue to be leading causes of death for adults in our country,” said Dr. Jason Foltz, chief medical officer, ECU Health Physicians. “High blood pressure is a leading risk factor of heart disease and stroke that can often be prevented or managed if diagnosed and treated properly. Our region experiences high rates of diabetes, stroke and heart disease, and the Target: BP program allows ECU Health to better help patients lower their blood pressure by putting proven knowledge and guidelines to work on a daily basis.”

ECU Health Physicians clinics achieving Gold Status in Target: BP for 2023 include:
- Firetower Medical Office – 1204 E. Fire Tower Road, Greenville
- Family Medicine Center Purple and Gold Modules – 101 Heart Drive, Greenville
- General Internal Medicine – 521 Moye Medical Center, Greenville
According to the American Heart Association, high blood pressure, or hypertension, is a leading risk factor for heart attacks, strokes and preventable death in the U.S. There are 121.5 million adults in the country living with hypertension – that is nearly half of all adults in the U.S. Unfortunately, less than half of them have their blood pressure under control, making both diagnosis and effective management critical. Heart disease is the leading cause of death both nationally and in the state. Meanwhile, stroke is the fifth leading cause of death in the U.S., yet is the fourth leading cause of death in North Carolina.
Target: BP is a national initiative formed by the American Heart Association and American Medical Association in response to the high prevalence of uncontrolled blood pressure. The initiative aims to help health care organizations and care teams, at no cost, improve blood pressure control rates through an evidence-based quality improvement program and recognizes organizations that are committed to improving blood pressure control.
“By committing to helping more people in eastern North Carolina control their blood pressure and reduce their risks for future heart disease and stroke, ECU Health is taking a key step to helping more people live longer, healthier lives,” said Yvonne Commodore-Mensah, PhD, MHS, RN, FAHA, Target: BP advisory group volunteer and associate professor at Johns Hopkins School of Nursing. “ECU Health’s participation in the Target: BP initiative shows its dedication to turning clinical guidelines into lifelines for patients and their families.”
Four students in the Brody School of Medicine at East Carolina University have been named to the 2023-24 class of the North Carolina Albert Schweitzer Fellowship (NCASF) program and will spend the next year working on projects that address social factors that impact health and health care. Their projects will be completed in part at ECU Health facilities.
They are part of a class of 29 North Carolina graduate students — including two other Brody students and two students in the ECU School of Dental Medicine — representing medicine, dentistry, physical therapy, occupational therapy, public health and law.
“Schweitzer Fellows are not given a project or told to address a specific health need,” said Barbara Heffner, executive director of the N.C. Albert Schweitzer Fellowship. “They follow their passion and the needs of the community to develop innovative approaches which fill gaps in our health care system.”
Schweitzer Fellows develop and implement service projects that address the root causes of health disparities in under-resourced communities, while also fulfilling their academic responsibilities. Each project is implemented in collaboration with a community-based organization. Schweitzer Fellowships include an intensive leadership component, with fellows working closely with community and academic mentors during their fellowship year.
The ECU Schweitzer Fellows working on projects through ECU Health sites are:
Miranda Freeman and Michael Burt, Brody School of Medicine

Miranda Freeman

Michael Burt
A.C. Reid Schweitzer Fellows
Academic Mentor: Dr. Rima Panchal
Site Mentor: Dr. Margaret Clifton
Site: Palliative care unit at ECU Health Medical Center and Service League of Greenville Inpatient Hospice
Freeman and Burt are developing an end-of-life companions volunteer program to provide compassionate end-of-life companionship to palliative care patients who do not have anyone able to visit them. Volunteers will receive basic inpatient and outpatient hospice training, participate in narrative medicine workshops and will become knowledgeable advocates for the role of palliative services in modern patient care.
Freeman, a fourth-year medical student and native of Eagle Springs, said her passion for the project comes from her father’s recent cancer diagnosis.
“I saw how incredibly important it is to have support and care during scary difficult moments in life,” she said. “End of life should not have to be something individuals go through on their own. This program aims at providing more support to those at the final stages of their lives.”
Burt, a fourth-year medical student from Williamston, said the project aims to bridge a gap for a vulnerable population that deserves support.
“One group of individuals who are often not appreciated in conversations about loneliness is those who are in hospice care,” he said. “There are unfortunately many people who find themselves alone as they approach the end of their lives, and we believe they deserve the option of compassionate companionship, outside of their health care team, during this time.”
Vaishnavi Siripurapu and Elisabeth “Ella” Whitfield, Brody School of Medicine

Vaishnavi Siripurapu

Elisabeth “Ella” Whitfield
Academic Mentor: Dr. Lisa Moreno
Site Mentors: Dr. Hannah Florida, Dr. Lauren Sastre
Site: ECU Physical Medicine and Rehabilitation Inpatient Unit
Siripurapu and Whitfield are launching a cardiovascular health intervention for patients at the ECU Physical Medicine and Rehabilitation Unit focused on individualized goal setting, nutrition education, behavioral health and community support.
Siripurapu, a second-year medical student from Mooresville, said her passion for the project comes from watching her father’s diabetes journey.
“After following his journey and realizing the impact that chronic cardiovascular disease has on many people in my rural community,” she said, “I decided to pursue a project in order to address this unmet need that has manifested in my own life.”
Whitfield, a second-year medical student from Durham, said the project will address continuity in support from the hospital to home.
“During their hospital stay, patients are provided with structure, nutritional counseling and convenient healthy meals, therapy such as physical and occupational therapy, and support from hospital staff. However, upon discharge, this support structure is removed, leaving patients feeling isolated and powerless in their circumstances,” Whitfield said. “With the status quo, patients have a difficult time creating lasting change. We hope to ease this transition for CVD patients, and prevent future re-hospitalizations, by providing an abundance of supportive measures during this gap in care. We want to support individuals in a holistic way and help to empower them to feel confident in their ability to take charge of their own health journey.”
The NCASF is funded through the Blue Cross and Blue Shield of North Carolina Foundation, Delta Dental of North Carolina, Duke University School of Medicine, ECU Brody School of Medicine, North Carolina Area Health Education Centers, North Carolina Central University School of Graduate Studies, University of North Carolina School of Medicine, North Carolina Oral Health Collaborative, UNC Office of Interprofessional Education and Practice, ECU Health, Wake Forest University Health Sciences and individual donors.
NCASF began in 1994 as a local chapter of the national nonprofit, the Albert Schweitzer Fellowship, and has trained more than 600 leaders in health care. Nationally, more than 4,000 U.S Schweitzer Fellows have served individuals and communities in need and are continuing to shape health care policy and provide direct service.
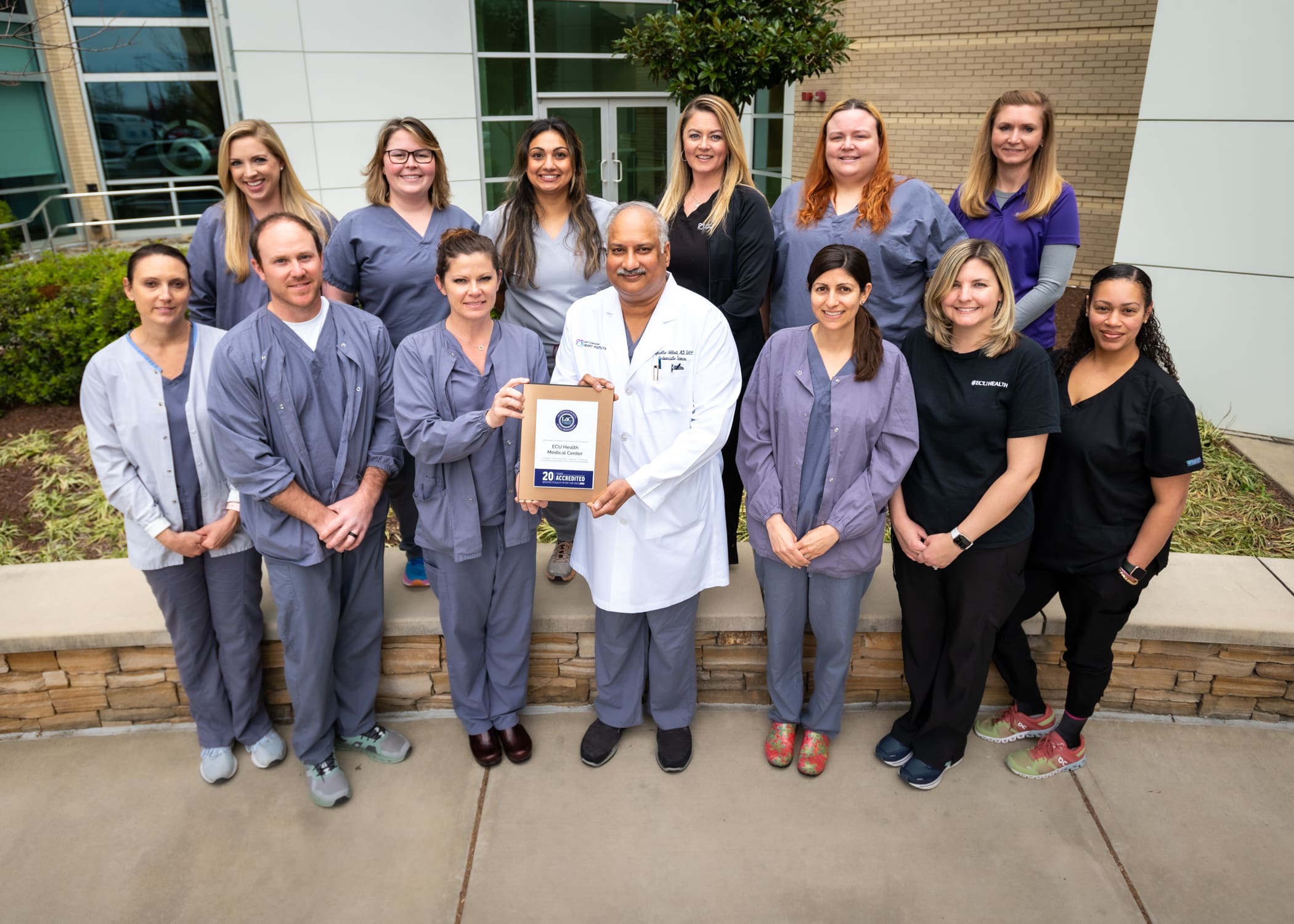
Greenville, N.C. – ECU Health Medical Center Echocardiography Laboratory (Echo lab) earned a 20 Year Bronze Accreditation Milestone for its reaccreditation and pediatric echocardiography reaccreditation by the Intersocietal Accreditation Commission (IAC). The Echo lab has also been granted a three-year term of accreditation by the IAC in Echocardiography in the areas of adult stress, adult and pediatric transthoracic and adult transesophageal.
Accreditation by the IAC means that ECU Health Medical Center Echo lab has undergone an intensive application and review process and is found to be in compliance with published standards, thus demonstrating a commitment to quality patient care. Comprised of a detailed self-evaluation followed by a thorough review by a panel of medical experts, the IAC accreditation process enables both the critical operational and technical components of the applicant facility to be assessed, including representative case studies and their corresponding final reports.

“ECU Health takes great pride in bringing state of the art, high quality care that’s close to home for eastern North Carolina.” said Dr. Dave Harlow, senior vice president of Allied Health at ECU Health. “ECU Health’s partnership with the Brody School of Medicine at East Carolina University allows us to provide world class training and technologies for clinicians and medical students alike which ultimately improves patient outcomes. These efforts are tailored to our mission of improving the health and well-being of eastern North Carolina, and I am proud of the teams that earned this reaccreditation and the effort it represents.”
A noninvasive ultrasound study called an echocardiogram is commonly used to evaluate heart structure and function and can detect heart disease or signs of serious conditions. According to the Centers for Disease Control and Prevention, heart disease is the leading cause of death for men, women and people of most racial and ethnic groups in the United States. On average, one American dies every 34 seconds of cardiovascular disease. Each year nearly 40,000 infants in the United States are born with a congenital heart defect, making it the most common type of birth defect. Congenital heart defects are also the most critical, causing more deaths during the first year of life than any other birth defect.
There are many factors that contribute to an accurate diagnosis based on echocardiography including the training and experience of the sonographer performing the procedure, the type of equipment used and the quality assessment metrics each facility is required to measure. IAC accreditation is a “seal of approval” that patients can rely on as an indicator of consistent quality care and a commitment to continuous improvement.
“Eastern North Carolina sees higher rates of chronic diseases including hypertension, diabetes and stroke, all leading to higher rates heart disease,” said ECU Health Medical Center Echo lab medical director Dr. Raj Nekkanti, who also serves as a professor in the Division of Cardiology and Program Director of the Cardiology Fellowship Program at Brody. “Having a high-quality, consistent Echo lab helps ensure accurate diagnoses and is instrumental in creating treatment plans for patients. Early diagnosis of heart disease can drastically improve outcomes for patients, highlighting the necessity of these types of services. We are proud to offer this high-quality care to a region that depends on it.”
East Carolina University’s postgraduate program in cardiac psychology creates professionals who are ready to help patients cope as they adapt to life-saving heart devices.
On the heels of marking its 15th year, ECU’s nationally unique program in clinical health psychology continues to gain momentum through positive patient outcomes — and national recognition.
The program is a collaboration between ECU’s departments of psychology and cardiovascular sciences that has yielded a nationally unique blend of academics and research. The model integrates training psychology doctoral students and cardiology fellows in cardiac clinics, a strategy that the program’s founder calls the best of both worlds.

“This is a success story from eastern North Carolina,” said Samuel Sears, program director and professor in the departments of psychology and cardiovascular sciences. “From a national landscape, this is an extremely unique program. Only at East Carolina do you have this kind of synergized, integrated, one-for-one engagement in the training of cardiologists and the training of psychologists. Our program is intending to lead the country in this.”
Sears established the training program in 2007 and collaborates with Rajasekhar Nekkanti, associate professor and director of the cardiology fellowship program at ECU and ECU Health, to offer ECU students an integrated program experience that spans clinical care, research and training.
“Dr. Sears and his colleagues have been able to accomplish what others have only talked about,” said Alan Christensen, professor and chair of the ECU Department of Psychology. “Their seamless integration of clinical psychology into a cardiovascular medicine setting is really a pioneering effort in implementing what I believe will prove to be a more effective approach to training, research, and caring for patients.”
The growing field of cardiac psychology focuses on providing psychological care that is an interdisciplinary, comprehensive care approach to cardiac arrhythmia patients and their families.
Depression and anxiety are common occurrences after cardiac events and can occur in as many as one-third of all patients. These conditions interfere with all aspects of recovery from daily rehabilitative planning, medication adherence, and the pursuit of quality of life.
“Cardiac psychologists help by validating the emotional experience of having a heart problem, and helping patients take the next steps in their recovery emotionally and behaviorally,” Sears said. “ECU Cardiology and Cardiovascular Surgery continue to innovate, and that allows our patients to survive. Here at East Carolina, we have the vision and program to address the patient experience and recovery process fully from a psychological and behavioral perspective. We integrate all the aspects of recovery and prepare trainees for the future of cardiac care.”
The program was highlighted in a 2022 edition of Health Psychology, a journal of the American Psychological Association. The article, “Cardiac Psychology Training in a Rural Health Care Setting: East Carolina Heart Institute,” was led by author Kayla Sall, a 2023 graduate of ECU’s clinical health psychology program. Doctoral students Ashley Griffith, Emily Midgette, Andrea Winters and Connor Tripp also co-authored the article with Sears and Nekkanti.
“We are very proud to publish in our field’s top journal,” said Sall, who begins a psychology internship at Brown University this fall. “The publication goes to show how unique our training experience is. It’s very rare to find cardiac psychologists that are located in cardiology.”
The Health Psychology article covers not only the program’s unique nature of intertwining science with practice, but also its ability to adapt to the COVID-19 pandemic by transitioning to using telehealth to serve patients in rural North Carolina. It also explores the health disparities in eastern North Carolina that impact cardiac patient care and progress.
“Cardiovascular health is one of the leading causes of death in the U.S.,” Sall said, “so being able to take that lens and apply it to the social determinants of health has been amazing, and it’s how we’ve been able to do what we do.”
Greenville native and ECU graduate Scarlett Anthony didn’t have to go far to find a program that offers world-class education and preparation that will help her make a difference in her home region and beyond.
“I chose ECU’s program because of the focus on health psychology and the intersection between psychology and medicine. We train alongside psychologists who are embedded in medicine, and our program provides us with exceptional training among various health care settings,” said Anthony, a doctoral student in clinical health psychology. “I chose ECU’s program because of the dedication to serving diverse populations of eastern North Carolina, and I am passionate about providing care to those who may not have access to health psychology services otherwise.”
Standards of practice

Sall led the writing team in detailing the ECU training program and its strong collaborations in cardiology. The article presents ECU’s program as a national model for ideal collaboration between cardiology and psychology training that enhances the clinical and research expertise of both groups.
The ECU cardiac psychology program is part of the APA accredited clinical health psychology program. This program has achieved national rankings over its 15-year existence and annually has an approximately 5% acceptance. Rob Carels serves as the director of clinical training for the clinical health program.
“The article confirmed that the ECU program is not only one of a kind, but it remains the model as programs and universities try to create this similar-type experience,” Sears said. “The reason it’s so hard to create the ECU experience is that it requires both physicians and psychologists accommodating very different mindsets and contributions with the shared goal of patient success first. Physicians can quickly implant a cardiac device. Psychologists can quickly assess and treat psychological concerns. But when these two sets of problems merge, we need shared expertise.”
The article also highlights the setting of ECU’s health psychology program, a rural area where the social determinants of health — including environment, economic stability, community context, education and health access — impact health and wellness on a greater scale.
“Being in eastern North Carolina, we have a very unique setting with our patient population in a rural area,” Sall said.
That context allows psychologists to better understand the behavioral and mental health of cardiac patients. Many patients seen by cardiac psychologists at the East Carolina Heart Institute include those who suffer depression after a heart attack or other cardiac event, those with atrial fibrillation (a-fib) and those who have recently been fitted with implantable cardioverter defibrillators (ICD) — devices similar to pacemakers that correct heart arrhythmias with a high energy shock that can feel like being kicked by a horse.
“I think that is what is so scary for patients; they agree to have this device implanted, they know it’s life-saving, but you don’t know when the shock is going to go off,” Sall said. “You may go the whole rest of your life without receiving a shock, so that’s where part of the anxiety and fearfulness comes in.”
In the program’s scientist-practitioner approach, providers on each side have a thorough understanding of the opposite discipline.
“I think that’s what’s cool about cardiac psychology — here we are with people presenting with medical conditions or health issues and we’re evaluating, diagnosing, treating emotional behavioral disorders within the context of health and medicine,” Sall said. “We’re not doing just one or the other, we’re doing these together.”
World expert in action
Sears is a highly productive researcher examining quality of life and psychological adjustment in patients with heart rhythm disorders and ICDs. He has published more than 200 articles in the medicine and psychology research literatures and has well over 11,000 citations. In 2021, Expertscape.com named Sears one of the top 50 experts and most prolific authors in the world on ICDs over the last 10 years, amongst the 27,847 authors on the topic.
“I’m involved in both the training of psychologists as well as the training of cardiologists, so we’re trying to make cardiologists better at patient psychology and psychologists better at understanding the cardiology, so it’s synergistic,” Sears said.
Sears travels the world presenting his research and lending his expertise to patient, family and physician groups.
In 2013, the UNC Board of Governors presented Sears with the O. Max Gardner Award, the highest honor bestowed to a faculty member in the UNC system for contributions to mankind.
“The O. Max Gardner Award changed me because I stopped looking for external validation about our achievements. I desperately wanted to make an impact on our patients, our students, our university, our state and beyond,” he said. “The award confirmed some of these marks, so I used my energies more efficiently on the work at hand. I am proud of the health psychology program and the cardiac psychology program that my colleagues and students have created. In terms of work, I am so pleased that many of our ideas about helping cardiac patients are broadly employed across many sectors in cardiology, not just where we started.”
The article in Health Psychology signals consistent success and upward momentum for the program, said Sears, adding that Yale University’s health psychology program is the only other such program mentioned in that edition of the journal.
“This is a 15-year-old program. We’ve established success,” he said. “This is not a great idea that’s going away. Great ideas happen all the time, but they’re not sustainable. This is a sustainable solution that has true outcomes.”
When it comes to patient outcomes, Sears is optimistic that the growing field of cardiac psychology will continue to yield hope and healing.
“We can’t fix all the health inequalities, but what we can do is help our patients make small steps to have better awareness of where there are a lot of possibilities and decision points, and connect them to other resources,” Sears said. “Yes, this is a hard mountain to climb. Let’s do this together.”
Doctoral student Zachary Force said students begin the program learning what clinical health psychology can offer the world — and how ECU is leading the way.
“ECU has always done things differently, and other institutions are starting to take notice. ECU’s cardiac psychology service has received national recognition as the only place in the country to receive specialized training in an area with increasing need,” he said. “ECU’s fighting spirit imbues its doctoral students with the resiliency needed to advocate for psychology within the medical field.”
Read more from ECU News Services
Wilson, N.C. – April 1, 2022 – Vidant Health is excited to announce the official opening of Vidant Family Medicine – Glendale, a primary care extension of Vidant Healthplex – Wilson, which is dedicated to providing high-quality primary care services to the community.
“Vidant Family Medicine – Glendale will fill an important need in the community by providing expanded primary care services to reach more patients,” said Rashanda Elam, service line coordinator, ECU Health Physicians. “Access to primary care, particularly in rural environments, directly benefits the overall health and well-being of a community.”

Vidant Family Medicine – Glendale, located three miles from Vidant Healthplex – Wilson, will offer treatment for a variety of issues including cold and flu-like illnesses, ear infections, allergies and other illnesses as well as offer Department of Transportation (DOT) clinical physicals and Nexplanon birth control implants. Importantly, primary care doctors screen for health conditions before any signs or symptoms may appear, which can both prevent and detect conditions early. When health conditions such as cancers, high blood pressure or diabetes are caught early, the chance of successful treatment is greater.
“The new clinic is close to the Healthplex, ensuring patients have convenient access to expanded, specialty care if they need it,” said Elam. “Vidant Healthplex continues to offer the same spectrum of specialty care including immediate care, heart and vascular care, neurological care, cancer care, dermatology, sleep medicine, endocrinology and more. By opening this dedicated primary care and family medicine location, we can provide a wide spectrum of care that helps meet the community’s needs.”
Vidant Family Medicine – Glendale will open 8 a.m. to 5 p.m. Monday through Friday for both children and adults. Deirdra Pearce, NP, Andrea Brooks, NP and Mallory Moore, NP will move from the Healthplex to serve at the new location. Current patients will be contacted directly with more information, or please reach out to the office with any questions and to schedule your next appointment.
The practice is located at 1704 Glendale Drive SW Suite C, Wilson, N.C. The clinic accepts walk-ins and appointments. To contact the family medicine practice, please call 252-246-8960 or visit the location page.