A pink ribbon is one of the most recognizable symbols in health care. This is because breast cancer, the disease for which the color represents, is the second most common cancer in women, affecting one in eight women. Breast cancer develops when an abnormal growth occurs within the breast tissue, typically caused by uncontrolled cell growth in the breast. These rapidly growing cells form a potentially cancerous lump or mass and can spread to other areas, including lymph nodes.
Breast cancer often presents as:
- A lump or mass in the breast
- A change in size or shape of the breast
- A change in nipple appearance, including a newly inverted nipple or discharge
“I encourage everyone to know and understand what their breast tissue should look and feel like so they’re aware of any potential change,” said Dr. Karinn Chambers, breast surgical oncologist, ECU Health and ECU’s Brody School of Medicine.
It is never too early to begin self-exams of the breast, according to Dr. Chambers. However, women should begin breast cancer screenings annually at age 40, according to the American Cancer Society. This consists of a mammogram, which is an x-ray of the breast.

Dr. Chambers also emphasized that everyone, including men, should be aware of their breast health.
“Anyone can get breast cancer,” said Dr. Chambers. “I have seen breast cancer in people of different ages, the young and the elderly. Men can also get breast cancer.”
While breast cancer in men is much less common than in women, the American Cancer Society predicts that about 2,710 new cases of invasive breast cancer will be diagnosed in men in the United States in 2022.
“When a man is diagnosed with breast cancer, typically they present with the same symptoms as women – a new mass or lump within the breast,” said Dr. Chambers. “The causes and risk factors of breast cancer in men and women are also very similar.”
Breast cancer has both unknown and known risk factors. While experts still do not fully understand all of what causes breast cancer, genetics and lifestyle play a role in breast cancer.
“We recommend that women and men with a close family history of breast cancer undergo genetic testing to understand if they have a mutation on either the BRCA1 gene or the BRCA2 gene,” said Dr. Chambers. “BRCA1 and BRCA2 genes prevent proteins from rapidly growing out of control, which can cause certain cancers. For those who have the mutation, we do recommend prophylactic bilateral mastectomies, or removal of both breasts, as a preventative means to try to reduce their risk of breast cancer.”
While genetic risk factors are out of an individual’s control, there are behavioral changes one can make to lower their risk for breast cancer. The first is eating a healthy diet and exercising.
“Obesity is a big risk factor for breast cancer, and the rise of obesity in our population has led to an increased risk of breast cancer,” said Dr. Chambers. “Excess alcohol use can lead to increased risk of breast cancer as well.”
Experts highly encourage individuals to discuss screening with their primary care providers to understand their own risk for breast cancer based on their hormonal history, family history, health and age. The early detection of breast cancer allows for less invasive treatments, a greater variety of options and a greater potential to prevent the spread of breast cancer. When a person is unfortunately diagnosed with breast cancer, there are a variety of treatment options.
“The treatment of breast cancer consists of local tools and systemic tools,” said Dr. Chambers. “Local tools like surgery and radiation target the tumor directly. Systemic tools such as chemotherapy and hormone therapy can reach cancer throughout the body and may be used if the cancer has spread beyond the initial breast tissue.”
The bottom line?
“To prevent breast cancer, an individual should first discuss screening with their primary care providers so that they understand when and how often to get breast cancer screening,” said Dr. Chambers. “The second part of that would be to understand their own risk for breast cancer. Lastly, always remember to practice self-exams and know what is normal for your breasts. If you experience any changes, notify your primary care provider.”
Early diagnosis and a variety of treatment options have largely increased the odds of curing and managing breast cancer. ECU Health continues to offer 3D mammography at ten convenient locations throughout our region. Patients can take advantage of ECU Health’s free online risk assessment tool, talk with a provider and schedule a screening that meets their needs.
To learn more, please visit ECUHealth.org/breast-cancer.
Greenville, N.C. – ECU Health donated Stop the Bleed Kits to public schools in Tyrrell, Currituck, Northampton and Halifax counties as part of its goal to distribute these life-saving resources to public schools across eastern North Carolina. These kits provide resources such as tourniquets, trauma dressing, compressed gauze, gloves and training for school staff in the case of a bleeding emergency before professional help arrives.
“ECU Health is excited to continue expanding our distribution of Stop the Bleed Kits in the counties we serve in eastern North Carolina,” said Erika Greene, pediatric trauma program manager for Maynard Children’s Hospital at ECU Health Medical Center. “Time is of the essence for traumatic injuries, and early intervention can save lives. In rural areas like eastern North Carolina where the distance between schools and hospitals may be greater, these kits enable school staff to treat children early, improving chances of better outcomes.”
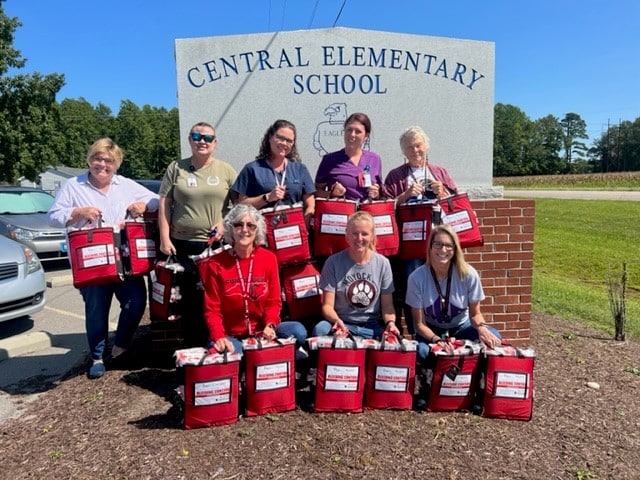
Stop the Bleed Kits are funded by Children’s Miracle Network with training provided by Maynard Children’s Hospital. ECU Health has donated more than 64 Stop the Bleed Kits to schools this year, with a total of 354 kits in 12 counties since the program started in eastern North Carolina. School nurses in each county help train staff to use the kits, which ensures more children can be treated with supplies that do not expire.
“We are thankful for the generous gift of Stop the Bleed Kits provided by Maynard Children’s Hospital for every school in Currituck County,” said Jennifer Solley, school nurse, Currituck County Schools. “An emergency in the school setting can occur at any moment. Stop the Bleed training and equipment in each school will equip the staff with the knowledge and tools needed to respond to any bleeding emergency. With these kits, we are prepared and able to reduce or eliminate the loss of life due to an emergent bleeding situation whether it be a single playground injury or a mass injury situation.”
Preventable blood loss is one of the most common contributing factors in trauma-related deaths. Approximately 40 percent of trauma-related deaths worldwide can be attributed to bleeding or its consequence. If bleeding is managed early, the chances of recovery and survival are much greater. The items in the kits help control the loss of blood, leading to positive outcomes for those who sustain injuries.
With an audience of more than 90 Brody School of Medicine at East Carolina University first-year medical students, leaders from ECU Health and Brody discussed the power of storytelling and narrative medicine during the 14th Annual Jose G. Albernaz Golden Apple Distinguished Lecture.
Narrative medicine is an increasingly popular technique that utilizes storytelling for health care providers to understand their patients as people and help process their own emotions around their work. At ECU Health, where compassionate care for patients and for the care team are foundations of how the organization meets its mission, the benefits of narrative medicine can make a difference in the clinical setting.
For first-year Brody students, the lecture provided an opportunity to learn about the value of narrative medicine so that they can apply it to their own education and future careers.

Dr. Christina Bowen, chief well-being officer of ECU Health, was once a first-year Brody student herself. In her opening remarks, she challenged students to take up narrative medicine early in their journey to becoming providers.
“The profession of medicine brings cases that will touch your hearts with much joy and sorrow. Write those stories down,” Dr. Bowen said. “These stories will be with you the rest of your medical career. Embracing the power and importance of these stories will support your emotional well-being and your growth into an excellent physician.”
Dr. Sharona Johnson, the nursing Advanced Clinical Practice administrator at ECU Health, served as the keynote speaker for the event. She said storytelling is key to understanding our humanity and helps leave a legacy for all people.
Dr. Johnson, who is a published author, is an advocate for narrative medicine – both to understand patients and as a well-being tool to get her own feelings down on paper.
“We’re learning that stories are important because we’re telling our stories,” Dr. Johnson said. “Physicians and health care professionals are writing books. We’re finding that our life has to have meaning. You can’t go through your life without thinking about, ‘Why am I here, what is the purpose, why is this patient sitting in front of me?’ It has to have meaning.”
Dr. Jason Higginson, chief health officer of ECU Health, said he received a written note from the first patient he gave a full clinical exam to in medical school. He said he can still picture himself in the exam room and remembers the patient frequently because of the heartfelt note the patient shared. He reflected that he wished he’d known more about narrative medicine as a young doctor so he could have captured more experiences like this from early in his career.
The relationship between ECU Health and Brody is important for many reasons. The opportunity for experienced providers to share valuable lessons with medical students in a clinical setting is one of the special benefits. Dr. Michael Waldrum, CEO of ECU Health and dean of the Brody School of Medicine, said the teaching offered at Brody and ECU Health stretches beyond the walls of the classroom.
“This was a really important lesson today for students and a great reminder for anyone already in health care,” Dr. Waldrum said. “Narrative medicine and storytelling help in many aspects. Brody School of Medicine concentrates on producing physicians that actually understand humanity. I’m really proud of that.”
Dr. Waldrum said that understanding humanity and human interaction is what led him to being a pre-med English major as an undergraduate.
Learning the humanities, he said, helped lay a foundation for him as a person and care provider. The lessons learned as an English major were reinforced in his first clinical rotation during his third year of medical school when a mentor told him to learn something from each patient, whether it is a personal or medical fact. He said that stuck with him and taking it into action paid off.
“That’s the story of humanity and history, understanding and respecting differences,” Dr. Waldrum said. “Stories are about history and looking backwards, but it’s also about creating an optimistic and positive future. That’s what we’re doing here: creating a new health system, evolving our school of medicine, always changing and making sure that we meet our communities needs and that we educate the best humans on the planet.”
The Albernaz Golden Apple Distinguished Lecture series is a great example of how ECU Health and the Brody School of Medicine collaborate to bring excellence in the clinical and academic setting for the betterment of eastern North Carolina.
It’s no secret prostate cancer is one of the most common cancers among men. In fact, nearly one in eight men will be diagnosed with prostate cancer in their lifetime. What many may not know is if caught early, prostate cancer can be easily treated and even cured. That’s why experts at ECU Health are urging men who have delayed getting a prostate cancer screening to return to their regular screenings to prevent advanced prostate cancer diagnoses.
The prostate, which only exists in men, is a walnut-sized gland tucked under the bladder and is involved in the reproductive process. The prostate can develop cancer and is one of the leading cancers diagnosed in men.
“We love to catch prostate cancer before there are any signs or symptoms. In order to do that, you need a blood test called a prostate-specific antigen, commonly known as a PSA blood test,” said Dr. Caroline Ames, ECU Health urologist. “Because the prostate is tucked up under the bladder, you may not have symptoms until it’s advanced.”
Dr. Ames says if prostate cancer grows large enough that it is causing symptoms, there may be blood in the urine or semen or difficulty urinating. More advanced stages can present symptoms such as bone pain, weight loss and swollen lymph nodes.
“Many of the people we take care of in eastern North Carolina are high risk for prostate cancer, especially African American and Latino men between the ages of 45 and 65,” said Dr. Ames.

African American men are more likely to develop prostate cancer and twice as likely to die from prostate cancer, as compared to non-Hispanic white men, according to the Office of Minority Health.
“This is likely due to genetics, lack of access to health care, general mistrust in health care and socioeconomic factors,” said Dr. Ames. “Those men with a family history of prostate cancer and men over the age of 65 who take one or two medications and are overall healthy, need a PSA screening every year.”
The screening process may look a bit different from what many may have experienced before. Dr. Ames, along with many other urologists, now do the blood PSA screening as the first line of screening. These providers will do a physical exam after the PSA screening indicates cause for concern. According to Dr. Ames, this method has brought in many more men for prostate screenings that may have not gotten one before due to anxiety or hesitancy of the physical exam. Men are encouraged to talk to their provider about the screening process.
“If you are diagnosed with prostate cancer, we will look at all of the treatment options available,” said Dr. Ames. “While some with low-risk disease may not need aggressive treatment, there are options available such as hormone therapy, radiation or prostate removal.”
The best treatment is prevention. Eating a healthy diet high in fruits and vegetables and low in processed foods and red meat can help reduce your risk of prostate cancer, along with quitting smoking.
“Obesity and smoking are two of the leading causes of prostate cancer,” said Dr. Ames. “Once you have been diagnosed and treated for prostate cancer, obesity increases the risk for the cancer coming back in the future.”
During the COVID-19 pandemic, screenings across the board significantly lowered. This is a significant concern amongst medical experts.
“Many people postponed their cancer screenings, and we are very concerned about that,” said Dr. Ames. “This increases the chance for a larger number of patients to be diagnosed with advanced or later stage cancers, including prostate cancer.”
The bottom line?
“You need to return to your cancer screenings, whether it be prostate, breast, lung or colon cancer screenings, especially if you skipped them during COVID-19,” Dr. Ames said. “Early detection can save lives.”
Resources
If you have experienced the pain, tingling or weakness that can occur with carpal tunnel syndrome, you are not alone. Carpal tunnel syndrome (CTS) is a fairly common condition which occurs when one of the major nerves to the hand, the median nerve which runs from the forearm into the palm of the hand, is squeezed or compressed as it travels through the wrist. Thankfully, what was once a complex treatment for CTS can now be accomplished more quickly and more effectively through new surgical interventions that reduce recovery times.
Milder symptoms of CTS can be treated with physician-directed home care, which may include wearing a wrist splint, avoiding daytime activities that may provoke symptoms, performing specific exercises and taking breaks from tasks to rest the hand. Medications may also be prescribed to relieve pain and inflammation.

In many cases, non-surgical treatments only provide temporary results, with symptoms eventually returning. Surgery typically becomes the recommended treatment option when this occurs.
“Carpal tunnel release surgery is one of my more common surgeries,” said Dr. Jeff Barwick, an orthopedic surgeon at ECU Health Beaufort Hospital, a campus of ECU Health Medical Center. “Traditionally, we would make an incision in the palm to access the tunnel and free the median nerve. The recovery would take anywhere from two weeks on the fast end to several months on the slow end. Also, during this recovery period, many patients would not be able to resume their normal activities using their hands due to pain and weakness.”
A modified procedure performed at ECU Health Beaufort called carpal tunnel release with UltraGuideCTR ™ can perform the surgery less invasively and with much quicker recovery time for the patient.
“Now, because of ultrasound guidance, we can essentially perform the same surgery but using a much smaller incision,” said Dr. Barwick. “We also come under the muscles of the hands instead of having to cut through them. The healing of the incision and the muscles has traditionally slowed down the recovery process. The ultrasound essentially serves as my eyes and allows me to see into the carpal tunnel with a very minimal incision. Having carpal tunnel release with UltraGuideCTR™ available at ECU Health Beaufort Hospital offers community members convenient access to the procedure and allows them to stay close to home. Patients can also enjoy a better quality of life. When people can’t enjoy life due to pain, numbness and weakness in the hands and wrists, this can be taxing to them mentally, emotionally and physically.”
Some of the benefits of this new technology include a faster recovery time as opposed to the weeks of recovery involved with traditional carpal tunnel surgery. Going underneath the muscles with a drastically smaller incision, rather than cutting, creates a more positive experience for patents and often times allows them to return to work and the activities they enjoy within three to six days.
According to Sonex Health, Dr. Barwick is the first physician in North Carolina to offer his patients both carpal tunnel release and trigger finger release with real-time ultrasound guidance. Providing this new and innovative technology for the local community is another example of ECU Health fulfilling its mission to improve the health and well-being of eastern North Carolina. For more information about carpal tunnel treatment options including the ultrasound assisted surgery, please call ECU Health Orthopedics – Washington at 252-946-6513.

Jamysen Howard during her NICU stay in 2010.
From premature babies to complex conditions, the Neonatal Intensive Care Unit (NICU) at James and Connie Maynard Children’s Hospital sees the youngest patients at ECU Health Medical Center and provides high-quality, compassionate care while looking after families throughout their NICU journey.
Along the way, many families find a community and support system around them as they navigate the experience.
Thriving 12 years later
Tonya Howard found out at her 11-week ultrasound that her daughter would be born with her intestines outside of her body, a condition called gastroschisis.
While baby Jamysen grew, plans were lining up to have a pediatric surgeon join the team at Maynard Children’s Hospital at ECU Health Medical Center just in time for Jamysen’s arrival. However, when she came four weeks early, the pediatric surgeon received emergency privileges and successfully operated on her just after her birth.
Tonya said the supportive care team helped her and her family immensely during their time in the NICU. While they took care of Jamysen, they also kept the family up-to-date and informed.
“The NICU nurses who, probably about four or five of them I still talk to, kept me up with Jamysen’s progress,” Tonya said. “I had two other children at home, so I’d go home and spend the night and when I’d get up in the morning, the first thing I’d do is call the NICU to see how she did that night. The nurses were the ones that took care of her and they were with her all night.”

Jamysen is now in 7th grade, excels in school and plays volleyball for her school and travel teams.
She also said the NICU community is very strong and has been happy to serve as a support to other NICU families, including one that experienced gastroschisis, just like Jamysen.
Today, Jamysen is 12 years old and thriving. Tonya said while they were told there was possibility Jamysen could experience trouble with physical and mental development, she is now an honor roll student and plays volleyball with school and travel teams.
“We’ve always told her that she can do anything she wanted to do,” Tonya said. “I was like, ‘before you were one day old, you’d already been through a five-hour surgery so you know what, you can do anything you want to do.’ And she’s done just that. She knows she’s tough, she’s never had much fear and she’s headfirst into everything and always has been.”
Jamysen frequently participates in Children’s Miracle Network events as well.
Tonya has a unique perspective on the Maynard Children’s Hospital as a former team member in the pediatrics department, including time before the Children’s Hospital was built.
“At one point the NICU was just one big room. When Jamysen was born, the NICU was what it is now and each baby had their own individual room,” Tonya said. “Everything from the beds to the Child Life
Sorry, no posts matched your criteria.
and now they’ve progressed to where the parents can even log on and see their babies when they’re not able to be there. We didn’t have that while we were there but that’s just amazing.”Rallying around Waylon

Waylon Denny is shown in a crib after having a tracheostomy.
On July 23, 2016, Waylon Denny was born at 23 weeks, weighing 1 pound, 4 ounces. He spent the first 298 days of his life at the Maynard Children’s Hospital, beginning with about four months in the NICU.
Following a surgery for young Waylon, he became sick and needed immediate intervention. His providers knew one treatment, called extracorporeal membrane oxygenation (ECMO), could be lifesaving.
“I mean, they all really rallied right around us,” Waylon’s mother, Sara, said. “They got the doctors and everybody in the PICU that had anything to do with ECMO to come down to look at him to see if he would be a candidate for ECMO. And I truly believe if it was not for his respiratory therapists and nurses fighting for him that day I really do not believe that he would even be here.”
ECMO is a treatment where blood is pumped out of your body and into a machine that removes carbon dioxide and then flows blood back to tissues in the body. One of the providers fighting for Waylon was Dr. Shannon Longshore.
“I remember Dr. Longshore telling us that in a baby his size, 23 weeks, he was already swollen,” Sara said. “Everything he had been through, she should not have been able to get the [tubes] in his neck. And I remember her telling us that she looked at the team in that room and told them that she was going to keep trying because we were two weeks away from going home. And she closed her eyes and told God if it was his will or for him to live, they would go in. Well, those [tubes] went in.”

Waylon started kindergarten this year.
Sara was a first time mom and said it was hard to know what questions to even ask. Luckily, she said, the doctors, nurses and respiratory therapists were there to help. They explained things to her and the family and checked on them frequently.
Six years later, the check-ins have not stopped, she said.
“We’ve had so many nurses, doctors, respiratory therapists, physical therapists and occupational therapists friend us on Facebook just so they can keep following him and see how he’s doing,” Sara said. “And then when we were able to go to the hospital before COVID, and we would go and visit the NICU and the PICU and everywhere where he had been.”
Waylon is six and starting kindergarten and has met every challenge he’s faced in his young life head-on.
September is NICU Awareness Month and Sara said that she and Waylon have NICU Awareness Day (Sept. 30) t-shirts that they wear each year and she’s looking forward to celebrating and recognizing the day once again with her miracle son.
Twins fight through NICU together

Twins Molly and Lucy Davis are shown during their NICU stay.
Owen and her husband Garrett Davis were expecting twins and enjoying a family vacation before welcoming the new additions to their family. But their vacation was cut short when Owen could feel something was not right and she went into labor at 22 weeks.
Molly and Lucy Davis came into the world each weighing just 1 pound, 9 ounces and were immediately placed in the NICU at Maynard Children’s Hospital. The twins were both fighting infections early on in their lives and experienced many tests, treatments, procedures and exams over their 128 days in the NICU.
Owen said they experienced the full range of the NICU rollercoaster during their stay, but they were comforted along the way by the supportive and caring team at the hospital.
“One of the biggest things that I remember were the nurses and our neonatologists,” Owen said. “We still keep in touch with them really on a daily basis. Some of our nurses babysit for us, which is really special. Just the people that we encountered throughout our long stay made it bearable.”
Along with the great support of care teams, Owen said some of her family’s closest friends came from their time in the NICU. She said it is a special bond and shared experience for families of NICU children.
Recently, Owen had someone reach out to her on social media saying their friend was about to have a child at 23 weeks and the two got in touch with each other.

The Davis family takes a photo at the beach.
“It’s really cool to have that connection and to be able to provide insight and support to other families going through what we’ve been through,” Owen said. “So I’ve been in touch with basically a stranger from across the country who saw our story and reached out for some guidance and just a listening ear to be able to bounce questions off of and support and vent. It’s hard to understand unless you’ve been through it.”
Being open with her family’s story has brought comfort to others and she’s happy that her twin daughters are beginning to understand their own story as well.
She said it’s important to her that Molly and Lucy know how strong they are and that their parents advocated and fought for them from the time they were born.
“It was super hard and trying, but it’s also their testimony and they understand that at 3 years old. It’s really two miracles that we were able to witness,” Owen said. “They know, as much as a 3-year-old can. We have their blessing beads, these little beads that they got for every procedure and every test they had, we have them hanging up on their beds and we have their first diapers that are about the size of a credit card. We keep two of those on our entryway table in our living room as a constant reminder of what they’ve been through.”
Owen said she has a video that she put together of her daughters’ NICU stay that shows up in her memories each September and serves as a reminder of the importance of the month for her family — and so many others.
Resources
Renovations to the Pediatric Intensive Care Unit at the James and Connie Maynard Children’s Hospital, known as the PICU, provided a special way to honor some of the bravest patients.
“I’ve had families who their child has spent a significant amount of time in the PICU and asked, ‘How can we leave my child’s legacy on the unit?’” said Child Life Specialist Chelse Cudmore. “And I saw a picture of a wave and I was like, you know, a wave really represents patient and families stays while in the ICU as well as represents grief.”
One ECU Health nurse, Lacey Boldyrev, knows firsthand the journey of a family in the PICU. Her son Thaddeus was transferred to Maynard Children’s Hospital shortly after his birth.
“He was born in Jacksonville at Onslow Memorial Hospital,” said Boldyrev. “We had had just the normal pregnancy, normal ultrasounds, nothing special. I went to go get him and they told me that I couldn’t pick him up and I had to go back to my room and that the doctor would call me there. So I went back to the room and I waited. And the pediatrician that was in the hospital that day, she called and she said, ‘Your son has congenital heart disease and we’re going to send him to Greenville.’ He passed away on Christmas Day, December 2015. And I just felt like after he was gone, that there was that big empty hole.”
In the year that followed. Lacey felt called to serve the medical field and to care for patients just like her son. Her first choice upon graduating from nursing school was the PICU at Maynard Children’s Hospital. The admiration is mutual with the child life team honoring Lacey and choosing Thaddeus’ legacy to represent those who came before.
Cudmore reflected on the wave wall selection process.
“As we were talking about, how could we make this a significant thing? And Lacey, having a child who spent a significant amount of time and would have absolutely qualified for the wall and then him passing as well, and then her that kind of motivating her to want to be a nurse and our PICU. I mean it was really no question about it,” Cudmore said.
“I was asked by the child life team if I would want to put that on the wall,” said Boldyrev. “And I was completely honored to do that. It’s just a little bubble that it means a whole lot to me.”
Resources
Watch more ECU Health News videos
Meet Clive, ECU Health Medical Center‘s resident canine.
“Currently, he’s working two days a week with us,” said recreational therapist and dog handler Kasey Shue. “Some mornings when we go through the hospital doors, he’s just like, on a mission. I have to be like, ‘Clive, wait, hold on, buddy. You’re like, ready to roll this morning’. So I think he knows what he’s here to do.”
It’s an assignment he’s well prepared to tackle.
“A service dog is specifically trained to do certain tasks for somebody with a disability,” said Clive’s owner and outpatient rehab supervisor Tanya Bowen. “So a therapy dog is basically to provide comfort and they have to be very friendly and outgoing because there’s a lot of people that want to pet them and touch them. They have to be calm. They have to like the interaction, the social interaction. So he’s kind of like a little combination of both.”
Clive’s skill set benefits patients in a number of ways, whether that’s assisting with physical needs or providing emotional support.
“We’ll partner up with a physical therapist or an occupational therapist and we’ll work on walking him if they’re working on mobility improvement,” Shue said. “We’ll work on throwing a ball if they need some hand strengthener. We’ll work on them being able to pick up a very small treat and hand it to him if they have fine motor limitations. We really try to incorporate him into whatever functional skills they are trying to learn to make their life easier when they get home. On the other side, many times we have patients that are depressed or anxious. They don’t like being in the hospital and he just provides that comfort.”
And his services are in demand at the bedside and beyond.
“He actually wears a vest that says, I’m friendly, please ask to pet me,” Shue said. “We absolutely encourage that because he is therapy for our patients, but he’s also therapy for the staff, the families.”
Resources
ECU Health Therapy & Rehabilitation
Watch more ECU Health News videos
At ECU Health, team members go above and beyond to form trusting relationships with patients and their families to better serve eastern North Carolina.
Over the last 14 years, Occupational Therapy Assistant Winnie Miller worked one on one nearly every week with Taylor Anthony, who is now preparing for his freshman year at the University of North Carolina Wilmington. Taylor is autistic and began receiving treatment from an occupational therapist when he was 3 years old.
First steps
Kim Anthony, Taylor’s mother, recalled the early days of her son working with an occupational therapist.

“He was my first child and had special needs,” Kim said. “I remember walking in and just being terrified – you don’t know what your future looks like, or his future, or will college even be an option.”
After about a year of working with a couple of other occupational therapists within the health system, Miller stepped in and began her treatment sessions with Taylor.
Miller said their work together started with the base steps – figuring out hand dominance, holding pencils, learning to write, forming letters and coloring within lines.
Kim said as Taylor reached school age, she’d be frustrated when hearing about things that people believed Taylor could not do. But she knew she could turn to Miller and her expertise to come up with a plan to help Taylor reach his goals.
“I would email her and be like, ‘I’m struggling with this’ and she would be like, ‘OK we’ll figure it out,’” Kim said. “She would have checklists for him and just everything. It was amazing. She was the biggest support system I had.”
Hitting their stride

As Taylor got a bit older they worked on how to tie shoes and other fine motor skills. Then it was on to processing your environment and communicating clearly, social aspects of life, how to drive, and other elements of college life and living independently.
Miller compared her role as an occupational therapist to being a coach, with the patient’s supportive family as the team.
“The coach can give suggestions and a play-by-play plan of what you need to work on, but we’re just a little snippet,” Miller said. “I’m only with him an hour a week. They, as a team, have to work on those skills 24/7. I knew they were doing their work at home and there was always going to be follow through.”
Taylor’s father Stephen Anthony, director of service line development for Women’s and Children at ECU Health, said Miller’s out-of-the-box thinking greatly benefited Taylor’s growth into the young man he is today.
Miller broke down the learning process, kept his steps very goal-oriented and stayed in frequent contact with the Anthony family along the way.
“She made it manageable; she made it like they were just going to visit with each other. It wasn’t like a clinical visit, it was just, ‘Hey let’s go in my office and look at some stuff,’” Stephen said. “Maybe they do some stuff on the computer, maybe they use the kitchen to make some eggs or something like that, safety skills with the oven. Stuff that nobody would ever even think of.”
Off and running
These visits also included working with Helen Houston, an occupational therapy driver rehabilitation specialist, who addressed Taylor’s fitness to drive, to ensure he could approach driving safely.
Stephen said Taylor took one test as he was approaching driving age that showed his reactions and reflexes were borderline to be a driver. Before he took a driving test, he was put through the same tests, which showed about 75 percent improvement thanks to his hard work. Now, Stephen said Taylor is just as good a driver as anyone and probably safer than most his age because of the work he’s done.
Taylor said he was thankful for his time with Miller and he’s excited to take all he’s learned to Wilmington.
“It has meant a lot,” Taylor said. “I’ve definitely learned many things. It also took a lot to learn from a different perspective. My family means a lot. They’ve done everything for me to be sure I’ll be the most prepared human being. They’ll know I’ve learned enough to make good decisions and they’ll be supportive of me no matter what.”
As Taylor prepares for his first year of college, one where he’ll also compete as a member of the UNC Wilmington Cross Country team, his family knows he is prepared for different aspects of college life, thanks in part to his work with Miller.
Miller said she loved working with Taylor and can’t wait to visit with him when he returns from school and hear about his college experience.
“He was always an hour a week that I looked forward to,” Miller said. “He always had a new question for me or something new that kept me on my toes and I didn’t know what was going to be the question of the day, what we were going to have to explore and figure out. I really enjoyed that challenge. I’ve loved every minute.”
Resources
Learn more about Therapy & Rehabilitation services at ECU Health.

For the Eastern Carolina Healthcare Preparedness Coalition (EHCPC), being ready is part of the job.
“What we have here is our field communications support truck,” said Matt McMahon, disaster services specialist with EHCPC. “This is essentially the heartbeat of our mobile field hospital.”
From trucks that double as mobile hospitals to coordinating evacuations or the deployment of medical supplies, the coalition remains on standby for when emergencies strike or networks go down.
“So, if a hospital loses communication, whether it be phone, radio or internet, we can come and support them,” McMahon said.
The coalition provides a critical line of support, whenever and wherever it’s needed most. As they prepare for hurricane season, they want you to do the same.
“We want people to be prepared, and starting a hurricane kit is the first step in doing so,” said Chris Starbuck, health care preparedness coordinator for EHCPC.
A basic kit includes important items, like water, food and other supplies to last several days. Ready.gov is a federal government website with helpful information about how to properly prepare for a hurricane. Creating a plan that meets the specific needs of your household and building an emergency kit that contains at least 72 hours’ worth of supplies can help you stay adequately prepared for a natural disaster like a hurricane.
“Put all your important documents together – marriage certificates, birth certificates, wills,” Starbuck said.
Another item for your hurricane prep checklist – help others plan, too.
“Work with your neighbors, your communities, churches, because if we can prepare them, we can make a more resilient community overall,” Starbuck said.
Resources
Hurricanes can form quickly. Take the time now, before a hurricane impacts our region, to educate yourself on how to prepare and respond. Below are helpful links for federal and state websites:
- Ready.gov – Hurricane Information
- Ready.gov – Make a Plan
- Ready.gov – Build a Kit
- ReadyNC.org
- ReadyNC.org – Emergency Alerts
- ReadyNC.org – Evacuation Routes
- ReadyNC.org – Know Your Zone
Watch more ECU Health News videos





